"Cynthya was our doula for the birth of our third child in April 2016. As this was my third birth, and I had been attended to by a doula at the first two, I knew that finding the right doula was crucial to a successful and satisfying birth." - Winter Wheeler-Young
When Your Water Breaks: AROM Labor Management
It is best to understand your options, and always weigh risk versus benefit. No matter whether you choose to have your water broken or wish to avoid having it done, be sure you are making your choices because you understand and are comfortable with the decision at hand.
“I think we should try breaking your water to help speed things up,” said the OB. This is a very common method of attempting to hasten a stalled or slow labor, or an induction of labor. It sounds promising, but does breaking the amniotic sac - a procedure known as “amniotomy” or AROM (artificial rupture of membranes) - always accomplish this?
Are there any risks associated with this intervention? Because this procedure is quite commonplace in American hospitals, here’s the scoop on some of the science, benefits, and risks surrounding this procedure.
So what exactly is the “bag of water(s)” or the amniotic sac?
It is a very thin, strong, membrane that contains fluid that surrounds your baby in the uterus. This creates a nice cushion for your baby to soften any jolts or impacts to the belly. It also helps maintain a constant temperature and allows for easier movement and growth of your baby.
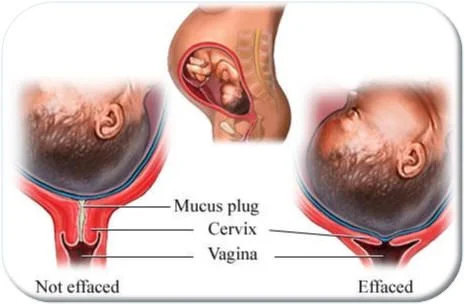
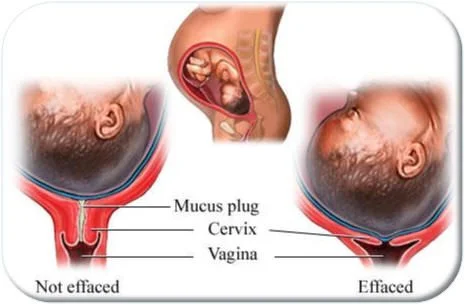
Why break it? The belief behind amniotomy in early labor, to induce labor, or to kick-start stalled labor before 6cm, is that breaking the bag of water using a small amniohook removes the fluid cushion between the baby’s head and the cervix, allowing more pressure to be placed on the cervix, resulting in faster dilatation of cervix. Often - whether artificially or on its own - the water breaking will encourage a rise in your natural oxytocin level, thus bringing on more contractions. Sounds great, right?
Maybe not. Opponents of AROM argue that the amniotic sac and fluid play an important role in protecting your baby against the stress of contractions. Imagine trying to squeeze/crack an egg inside a filled water balloon using pressure from your hands around the balloon.
Every time you squeeze, the squeeze is translated to pressure across the surface of the egg and it can move down and around as needed. Same concept with baby and their umbilical cord. That fluid can also make it easier for your baby to maneuver, should any additional maneuvering be necessary.
“Your intact amniotic sac can actually help with thinning and dilatation of the cervix.”
But what about the whole speeding up labor thing?
Although amniotomy can help shorten labor by one hour according to the American Pregnancy Association if done at the appropriate time, your intact amniotic sac can actually help with thinning and dilatation of the cervix as well, thanks to the water in front of baby’s head creating even pressure across the cervix. So leaving everything alone and letting your body do it’s job can also shorten your labor versus starting interventions that may not necessarily be needed.
What’s this about risks?
As with everything in life, there are also risks associated with artificially rupturing the membranes. These can include:
A prolapsed cord. This is when baby’s umbilical cord slips past the head into the vagina, cutting off circulation to baby significantly, resulting in an emergent c-section.
Risk of infection is also a problem. For this reason, most providers won’t let you labor too far past 24 hours after your water breaks or is broken and will suggest a c-section if your water is broken and you are not ready to push the baby out.
Another possible risk can be with the baby’s heart rate. Without the cushion of the fluid, it can be harder to un-squish an umbilical cord or placenta that is thought to be causing a drop in baby’s heart rate.
Also worth noting; a common side-effect of AROM is a significant increase in the intensity of what you are feeling, and are more inclined to ask for pain management or epidural.
That last one is not a true “risk” factor (and I myself have been a fan of the epidural) but for those who wish to avoid medicinal pain management and intervention domino-effect, it can make sticking to that choice much more difficult.
So no AROM ever, right??
WRONG. There are exceptions to almost everything in labor, and this is no different. If your baby is showing signs of extended distress and the medical staff are unable to get an accurate reading on the external monitor, it may be necessary to apply an internal monitor to the baby’s head in order to monitor baby’s heart rate without signal loss to ensure the heart rate stays stable. This is a situation where modern medicine and interventions shine and truly help protect baby and mother.
“The evidence showed no shortening of the length of first stage of labor and a possible increase in caesarean section.”
For those who skip to the end of these long posts to get the short version...Providers often suggest AROM to “speed things up” or “bring on labor.” However, a recent Cochrane review of 15 studies involving 5583 women states that “the evidence showed no shortening of the length of first stage of labor and a possible increase in caesarean section. Routine amniotomy is not recommended for normally progressing labors or in labors which have become prolonged.” The World Health Organization also reviewed the findings and supports that recommendation.
This is not to say it doesn’t ever help. It is simply best to understand your options, and always weigh risk versus benefit. No matter whether you choose to have your water broken or wish to avoid having it done, be sure you are making your choices because you understand and are comfortable with the decision at hand.
Related posts: How To Avoid Routine Medical Interventions 5 Reasons to Hire a Birth Doula 5 Labor Tools for PartnersHow To Avoid a C-section Without Changing Hospitals For Less Than The Cost of a Latte A Day
Get dependable support for less than $5 per day of your pregnancy. Think about that. Then think about the cost of a c-section and an extended hospital stay. Hiring an experienced doula who works well with your care providers WILL SAVE YOU MONEY.
Do you know how to avoid the primary c-section? Hire a doula.
The American College of Obstetricians and Gynecologists (ACOG) backs this claim. An excerpt from their website:
"Today, approximately 60% of all cesarean births are primary cesareans. Although cesarean birth can be life-saving for the baby and/or the mother, the rapid increase in cesarean birth rates raises significant concern that cesarean delivery is overused without clear evidence of improved maternal or newborn outcomes."
Read ACOG's full article published March 2014: Safe Prevention of the Primary Cesarean Delivery, which discusses ways to decrease cesarean deliveries, including:
Allowing prolonged latent (early) phase labor.
Considering cervical dilation of 6 cm (instead of 4 cm) as the start of active phase labor.
Allowing more time for labor to progress in the active phase.
Allowing women to push for at least two hours if they have delivered before, three hours if it’s their first delivery, and even longer in some situations, for example, with an epidural.
Using techniques to assist with vaginal delivery, which is the preferred method when possible. This may include the use of forceps, for example.
Encouraging patients to avoid excessive weight gain during pregnancy.
One of the main points is to use continuous labor and delivery support:
"Published data indicate that one of the most effective tools to improve labor and delivery outcomes is the continuous presence of support personnel, such as a doula. A Cochrane meta-analysis of 12 trials and more than 15,000 women demonstrated that the presence of continuous one-on-one support during labor and delivery was associated with improved patient satisfaction and a statistically significant reduction in the rate of cesarean delivery (111). Given that there are no associated measurable harms, this resource is probably underutilized."
“Approximately 60% of all cesarean births are primary cesareans.”
At the hospital, laboring families aren't truly supported during childbirth unless they have a doula present. Care providers are quite busy and frequently enter and exit the room leaving you unattended while they are busy with other patients. Our birth doulas stay by your side and provide support when you need it most!
Still wonder if doula support is necessary? Research your hospital's c-section rate - many metro hospitals are WELL ABOVE the national average of 32.2%. Afterwards, watch The Business of Being Born, a documentary "eye-opener" about birth in America.
Simply put, our team helps you obtain your true childbirth options so you can have a great labor and birth experience.
For less money than you'd spend on a latte a day, you can hire an experienced labor doula.
Get dependable support for less than $5 per day of your pregnancy. Think about that. Then think about the cost of a c-section and an extended hospital stay. Hiring an experienced doula who works well with your care providers WILL SAVE YOU MONEY.
Many of our clients use their HSA/FSA debit cards to pay for childbirth services such as classes and doula support. Our agency includes our NPI number and taxonomy code on our order confirmations so you may attempt reimbursement from your insurance company or HSA/FSA accounts.
You should also note that we offer eGiftCards. If you receive a gift card after to you after you've paid, you'll be refunded the amount to the credit card used to reserve services through our website.
“For less money than you’d spend on a latte a day, you can hire help from an experienced labor doula.”
You'll remember your birthing experience forever. I wish you and your family a healthy and happy birthday.
Be well,
Cynthya
Click to visit http://www.lamaze.org/p/cm/ld/fid=160
Reference: Safe Prevention of the Primary Cesarean Delivery http://www.acog.org/Resources-And-Publications/Obstetric-Care-Consensus-Series/Safe-Prevention-of-the-Primary-Cesarean-Delivery
Vaginal Exams Don't Predict Labor
Clients often misinterpret the residual symptoms of a vaginal exam for signs of labor starting on its own.
Beware! Around your 39th week of pregnancy, your OB or midwife will offer or expect you to have a vaginal exam. You should know these exams do not determine when labor will begin but do introduce bacteria, may cause bleeding and cramping, and risk premature rupture of the membranes, which could force an induction if labor doesn't begin within 24 hours.
"Clients often misinterpret the residual symptoms of a vaginal exam for signs of labor starting on its own." - click to tweet!
Once a client called me in tears stating that during an exam at her week 41 appointment, her OB "stripped her membranes" without her permission "to get things going." Ouch!
Unless you are in labor or about to be induced, knowing your dilation or effacement is not helpful. Many clients experience the early stage of labor for days (even weeks) or are a few centimeters dilated without contractions and it doesn't amount to much. Bottom line is: it may hurt, cause issues, and isn't helpful so why endure this highly inaccurate assessment?
Labor is divided into four stages
No one can predict when your body will begin labor. As a reminder, the stages of labor and what to expect for each are below.
Stage ONE is further divided into three phases:
Phase I: Early labor also called the latent phase.
Phase II: Active labor (5cm or 6cm dilation to 8cm)
Phase III: Transition (8cm dilation to 10cm or "complete")
Stage TWO: also called the pushing stage.
Stage THREE: the birth of your placenta.
Stage FOUR: the hour after birth.
For an overview of labor and birth with suggestions for progress and comfort, keep this webpage linked from your phone. To limit the amount of interventions throughout labor and birth, review our 7 part series, How To Alleviate Fears and Manage Labor Pain. To help you find out if your care provider is practicing within the current guidelines, read ACOG’s Committee Opinion, and ask your doctor what you can expect in the possible scenarios and how they will support your goals for baby’s birthday.
Stay in the know
The Happiest Doulas maintains a Pinterest board, Labor & Birth Support; Tips from Doulas, Midwives, and Educators. Follow it for more labor and birth tips from trusted resources around the world.
Stay well,
Cynthya
Related articles:
Avoid Routine Medical Interventions
Episiotomy and C-section Rates
AROM: To Break or Not To Break2 More Reasons You Don’t Need an Induction
No two pregnancies are the same (even within the same body), no two labors are the same; there are so many factors that play into a pregnancy and her subsequent labor and birth.
by Lauren King, Registered Nurse, Certified Lamaze Educator, and DONA Labor Doula
What is the average size of a baby born in America? Would you guess 7 pounds? Maybe 7 and a half? Eight pounds. Eight pounds is the average size of babies born in America. That means some (lots!) of babies are bigger than that – and many babies are smaller than that. Genetics and mom’s lifestyle, among other things, play a huge role in how big you grow your babies. I’ve seen babies born vaginally that weighed over 10 pounds! I’ve heard stories of babies just as large born vaginally with no pain medication! It’s certainly not impossible. (Maybe not necessarily the most pleasant thought… but not impossible!) Do you know how much amniotic fluid is adding to your weight? Well, not much honestly, but if you’re around 34 weeks, you have now reached the peak amount of amniotic fluid at about 800 mL. From 34 weeks on, amniotic fluid levels will gradually decline. Read on to learn why this matters.
Some doctors suggest an induction for “big baby” because they believe it decreases the chance of a shoulder dystocia (difficulty delivering the shoulders) or the need for a cesarean due to the baby being too large to fit through the pelvis. However, research shows this is simply not true. The risk of shoulder dystocia is relatively small – and it’s impossible to predict who will have a shoulder dystocia. Furthermore, for a doctor to suggest a woman to induce for this reason, the doctor must assume the ultrasound is accurately assessing the size of the baby. Next time a late-pregnancy ultrasound is recommended to you to assess fetal size during your pregnancy, ask your doctor or the sonographer how accurate it is. If they tell you the baby “might” weigh about 8 pounds, please know they can be off by as much as 2 pounds either direction. There is a HUGE difference between a 6 pound baby, an 8 pound baby, and a 10 pound baby. I have seen elective c-sections performed on first-time mothers due to “possible macrosomia” (big baby), only to discover the baby weighed LESS than 8 pounds.
I often tell people that things in labor and delivery can be very dynamic. The more I think about it, the more I realize how true that statement is in so many ways. No two pregnancies are the same (even within the same body), no two labors are the same; there are so many factors that play into a pregnancy and her subsequent labor and birth. Another dynamic aspect of pregnancy? Amniotic fluid. As I mentioned above, the amount of amniotic fluid peaks at about 34 weeks, reaching around 800 mL, and gradually declines to around 600 mL by 40 weeks. However, there are many factors that can play into these numbers. The baby, the mother, and the sonographer measuring the amniotic fluid can all affect the actual or perceived level of fluid.
The baby constantly circulates the fluid by inhaling it, swallowing it, and then releasing it through the urinary tract. Near term, the baby swallows more and urinates less often, thereby holding more fluid at any given time. Other baby-driven factors include: post-term (past 42-weeks), birth defect, or problems with the kidneys or urinary tract.
If you are dehydrated, such as in the coming summer months especially, if your water is broken, or if the placenta is no longer functioning properly, you may be diagnosed with low amniotic fluid. Some things you may try to increase amniotic fluid levels include drinking more water (at least 2-3 liters a day) and laying on your left side during an ultrasound when measuring fluid levels. Other factors that can play into an inaccurate reading include too much pressure on the ultrasound transducer, floating particles in the fluid, and an obese mother. Yes, “low amniotic fluid” could be a sign of a health issue and can be a medical reason for induction, but ask your doctor what their specific concern is before agreeing to induction simply for “low amniotic fluid.” Furthermore, you may wish to have a reevaluation in a couple days. Drink lots and lots of water, and when you return for another ultrasound (hopefully by the same sonographer!), if the fluid level is still low, or has decreased further, then you may wish to discuss the next step with your provider. If it has increased, then you might have saved yourself from an unnecessary induction! For a brand new diagnosis of “low fluid” without any other known cause, you may be better off to wait.
"What I have heard, and what I suspect it ultimately boils down to, is for one thing, doctors are human." - tweet this!
So, knowing all of this, why do doctors recommend things that are not backed by research or ACOG? My honest answer is: I don’t know. What I have heard, and what I suspect it ultimately boils down to, is that for one thing, doctors are human. Meaning: doctors want convenience and easy and predictable and good ratings. What? Good ratings? Exactly. Doctors and hospitals have a business to run. They have to keep their patients happy to keep them coming back for subsequent care! And businesses are consumer-driven. How many times have you heard that you can’t treat a viral infection with antibiotics? And yet, when a patient goes into a doctor’s office, demanding something to be done about their illness, they just might walk out with an antibiotic prescription in hand. Same thing with inductions. When a patient begs, pleads, whines, and complains about all the aches and pains, and difficulties of pregnancy, their doctor wants to appease them. No, not all doctors act this way, but the ones that do are the ones contributing to the problem and making it “okay” for other doctors to do the same. Although, I have to say – it’s not ALL the doctors’ faults. We, as women, as mothers, as consumers are just as much to blame. If I walk into my doctor’s office, demanding an induction – all the while, knowing all the risks of doing such – my doctor doesn’t want to lose me as a customer, so he agrees.
You Have More Power Than You Know
On the flip side, if more women – more consumers – are asking their doctors to allow their bodies to go into labor naturally, they will stop suggesting and allowing for non-medical inductions. If more women are getting educated on their options and on the pros and cons of such procedures, and refusing inductions for the sake of convenience, doctors will follow suit. Ultimately, they want to make their customers happy.
For more information on inductions, please visit MedLine Plus, American Pregnancy Association, and the Adventures of a Labor Nurse.
"Amniotic fluid peaks at 34 weeks, reaching around 800 mL, and gradually declines to around 600 mL by 40 weeks." - tweet this!
Related articles:
Knowing Your Options Is Vital To Your Labor And Birth
How To Avoid a C-section Without Changing Hospitals
6 Comfort Tips For NOT Breastfeeding
So You Need An Induction, Eh?So You Need An Induction, eh?
I believe women (actually any person) should be able to whole-heartedly trust their doctors. We want to believe our doctor is doing what is in our best interest – and they should be.
by Lauren King, Registered Nurse, Certified Lamaze Educator, and DONA Labor Doula
Photo By BirthYearBook
I feel the need to provide a disclaimer before I delve into this topic. I am not saying all doctors, midwives, or other medical staff are bad. There are definitely a lot of really great medical personnel out there. But just like anything in life, there are always a few bad apples.
I believe everyone should be able to whole-heartedly trust their doctors. We want to believe our doctor is doing what is in our best interest – and they should be. But I don’t think it’s a secret that there are doctors that sometimes do things in their own best interest. The question is: how do you know? As a non-medical person, how does one know their doctor is top-notch, and not suggesting every intervention, hoping for another nickel in their pocket, or hoping to be out on the golf course in an hour?
Of course, the obvious response here is: talk about your options with your doula from The Happiest Doulas, and we will do everything we can to help you achieve the beautiful birth you want and deserve. But equally as important is to be educated. You don’t need a nursing degree or a medical license to make important medical decisions, but you do need at least a pretty basic understanding of some of the top decision areas. And for everything else, ask lots of questions. Specifically, discuss the B-A-R with your provider: benefits, alternatives, and risks. When discussing pros and cons about procedures (especially induction) a great question for your provider is, “What research do you have about that topic?” or, “Where can we get more research-based information about that to help us make a decision?”
I’ve written before about inductions, but this is a topic that comes up a LOT in my classes. Plus, it’s the topic that really gets me started, gets me up on my high horse, my soap box… and it is hhhaarrrddd for me to get off it! “My doctor wants me to have another ultrasound next week because the baby is measuring big,” – and as a bonus to that one, “And if I don’t deliver by my due date, the doctor wants to induce me.” “My doctor said my amniotic fluid level is low.” “My doctor told me I need an induction because I conceived through IVF.” Ok, well, I don’t actually know what the literature says specifically about IVF, but just in my personal OPINION, it doesn’t make sense to me.
"I whole-heartedly believe in inductions for medical reasons for mom or baby’s health." - tweet this!
Let’s talk about the reasons for induction, though. There are actual medical reasons for induction, and I whole-heartedly believe in inductions for medical reasons for mom or baby’s health. What I don’t believe in is disguising a convenient induction in medical terminology. Here are some medical reasons for induction, according to ACOG: pregnancy that continues 1-2 weeks past the estimated due date, high blood pressure, uncontrolled gestational diabetes, an infection in the uterus, or a baby who is not growing properly (IUGR). This list is not completely exhaustive, but “big baby” and even “low amniotic fluid” (by itself) are not included in the list of medical reasons for induction.
I’ll discuss those two things in a later post, but for now, let’s discuss induction for postdates (going past your due date). Do you know what “EDC” or “EDD” stands for? Both start with E for estimated. (EDC stands for “estimated date of confinement”, in case you didn’t know.) A point I made in one of my classes recently was this: do you always have a 28-day cycle? Do you know, for a fact, that you ovulated on day 14 when you got pregnant? Do you know, for a fact, the exact date you conceived? (Ok, so some can truthfully say ‘yes’ here.) So, I went on to say: Did you all walk at 12 months? Did you all crawl at 7 months? Did you all roll over at 3 months? My point is that just as we all grow and develop at different rates Earth-side, so too do our babies grow and develop at different rates in the womb.
Due dates are calculated based on an archaic formula, called Naegele’s Rule, which assumes every woman has a 28-day cycle. Even then, the man behind Naegele’s Rule, Frederich Naegele, was not the original “inventor” of “how to estimate the length of human gestation.” It was an 18th-century professor of botany and medicine, Hermann Boerhaave, who developed the formula. Am I the only person who thinks this whole business of calculating a due date deserves a little more visitation by the research and medical community?!
Many Are Mislabeled as "Post-Term"
I do a lot of reading to keep up with the newest information. One of my favorite places to get information is from Evidence Based Birth. Rebecca Dekker, the author, just published a very extensive article on the evidence for inducing for going past your due date. She touches on Naegele’s Rule as well, but one thing she wrote really struck me. She wrote, “using the LMP [last menstrual period] to estimate your due date makes it more likely that you will be mislabeled as “post-term” and experience an unnecessary induction.” The reason for this is just as I stated above: not everyone’s cycles are cookie-cutter perfect! Even if a woman does ovulate on day 14, if she conceives that month, the embryo may not implant for several days! I was so thrilled for this article to come out, I wish everyone could take the time to read it word-for-word; however, I realize it is lengthy. I encourage you to skim it, and if nothing else, read the section “What’s the bottom line?” found at the end of the article.
"If a woman ovulates on day 14, and conceives that month, the embryo may not implant for several days." - tweet this!
So that you have more time to read that very important article, I’ll go ahead and end now. I hope this has given you some valuable information and resources. Next up, I’ll discuss why doctors induce for “big baby” and low amniotic fluid, so come back soon!