"Cynthya was our doula for the birth of our third child in April 2016. As this was my third birth, and I had been attended to by a doula at the first two, I knew that finding the right doula was crucial to a successful and satisfying birth." - Winter Wheeler-Young
Labor Tips for Birth Partners
If you've skipped taking a childbirth class during pregnancy, your partner may feel unprepared and need additional tools to support you during labor. Read Cynthya's 7 points to her clients.
As your due date approaches, it's completely natural for your partner to feel some anxiety regarding how they can best support you during the labor process. To help ease their uncertainty, I’ve compiled a helpful list of suggestions to guide them through it!
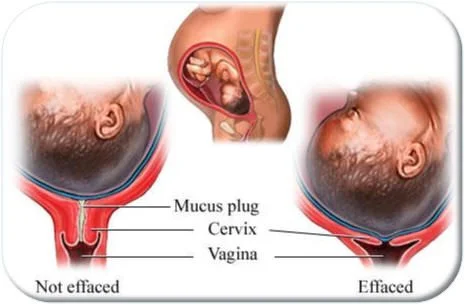
For instance, in early labor, taking a long, warm bath can be incredibly soothing, as it can relieve tension and ease anxiety. This suggestion is primarily meant for the laboring patient; however, if your tub is spacious enough, it can become a wonderful, relaxing experience for both of you to share.
The latent phase of labor is typically the longest stage of the process and can often wax and wane over time. It’s a great idea to take it easy during this time. Try to rest as much as possible between contractions and allow labor to progress at its own pace. Every minute of sleep that you manage to get will help to ward off future fatigue during the more intense active and pushing stages ahead.
It might be best to save the use of a shower for when you are at the hospital, as it may provide effective pain relief and help facilitate the progress of labor. For an optimal birth experience, explore additional tips here on how birth partners can provide effective and compassionate labor support.
How Taking a Childbirth Class May Help Prevent Birth Trauma
You go to one baby shower and inevitably, you start to hear the worst of the worst birth stories. “Did you hear about Kim’s birth? She pushed for FOUR hours and the baby was 11 pounds. Imagine. that. tear.” Everyone squirms.
by Megan Ciampa, Birth Boot Camp Childbirth Instructor
You go to one baby shower and inevitably, you start to hear the worst of the worst birth stories. “Did you hear about Kim’s birth? She pushed for FOUR hours and the baby was 11 pounds. Imagine. that. tear.” Everyone squirms.
“Andrea had to have an emergency c-section. She was induced and the baby’s heartbeat decelerated and they needed to deliver the baby immediately. Andrea’s blood pressure dropped and it was really scary. They said she almost died.”
Or, still, even worse:
“She asked for no episiotomy but the doctor insisted and cut her right before the baby was born. She had a 4th degree tear. Healing from that was the worst. She’s afraid to have another.”
While some of these stories may sound like just another unfortunate birth story, some of them are legitimate birth trauma. There is a term, called “obstetric violence,” that, on its surface, seems implausible. Obstetricians are all about bringing new life into this world; how could one be violent?
But when abuses bring with them “loss of autonomy and the ability to decide freely about their bodies and sexuality,” there is a price women pay at the hands of their care providers [Law on the Right of Women to a Life Free of Violence, supra note 13, art. 15(13)].
We know this does not characterize all or most OBs. But in the United States, in 2018, there are still too many women who experience birth trauma and feel more like a vessel of a person delivering a baby, and not like a human themselves.
“When you do not expect to have a problem with birth and then it happens, there can be long lasting psychological scars.”
Experiences such as these can have unfortunate consequences. Of course there’s the physical pain and recovery one must heal from. There’s also psychological and emotional recovery one hopes to experience as well.
In an article for The Atlantic, Ilana Strauss recounted stories of women who experienced post-traumatic stress disorder (PTSD) after giving birth. Not to be confused with postpartum depression, postpartum PTSD can be characterized by “hyper-vigilance, intrusive memories, flashbacks, severe emotional distress, irritability, trouble sleeping, and nightmares,” as is explained by Anastasia Pollock, a therapist who specializes in treating trauma.
Strauss also explained that the theory behind women who develop postpartum PTSD is complicated, but it often has to do with expectations. When you do not expect to have a problem with birth and then it happens, there can be long lasting psychological scars.
So… what does one do? How do you appropriately create your expectations?
Aside from talking to a wide range of women who have given birth before you and hearing their experiences, another very practical thing you can do is actually quite simple: take a childbirth class!
Not all childbirth classes are created equally, so do your research on with whom you study. What all is covered? Policies and procedures of the hospital? What meds you’ll be given? It’s important to discuss who your care provider is, and what his/her track record is for vaginal vs. cesarean deliveries. It’s also important to know your hospital or birth center’s policies and statistics. Even Consumer Reports is reporting on this. Read CR's article here.
To see Florida's c-section rates from 2016 and 2015, take a look at this spreadsheet from Florida Health Finder (source linked below). Check your state’s c-section rate here.
What else would you cover in a childbirth class?
In our Birth Boot Camp series, Training for an Amazing Hospital Birth, we discuss EFM or electronic fetal monitoring, the use of IVs, frequent vaginal exams and your care provider and/or hospital’s VBAC (vaginal birth after caesarean) policies.
We look back on the history of birth in this country and how it continues to impact the birth experience today. We discuss the physical and emotional happenings of labor and arm both mom and her partner to navigate it successfully. We share the stages of labor, including pushing and what positions are helpful and how the birth partner can help.
We educate on ways to avoid a cesarean, and how to feel at peace with one if needed. And perhaps most importantly, we arm you with the tools and knowledge you need to ask informed questions as you plan your birth and postpartum.
Taking a birth class does more than just show you how a baby is born. It shows you how amazing your body is, and how it’s your body, and how you can have a say over what happens to it. It encourages you to find and work with care providers who honor you and that process and respect your baby and you.
Sources:
https://scholarship.law.duke.edu/cgi/viewcontent.cgi?referer=&httpsredir=1&article=3924&context=dlj
http://www.floridahealthfinder.gov/researchers/QuickStat/cesarean-buffer.aspx
Related articles:
Positivity, Positions and Personal Support
5 Labor Tools for Partners
Postpartum Expectations and Must-have ItemsIs Waterbirth Safe? What are the benefits and risks for mothers and babies?
Our team has seen the beneficial effect of hydrotherapy use for labor and when clients give birth in the tub. The warmth of the water, the added buoyancy, with the addition of pouring water down the back or tummy, always adds a measure of comfort throughout labor and birth.
How To Have An Easy and Relaxed Labor
As labor doulas, we have seen the beneficial effect of hydrotherapy use during labor and while giving birth in a tub. We often suggest to clients that they take a long, warm bath in early labor to slow down contractions and relax the uterus enough so that sleep becomes possible. Once a strong pattern of contractions has been established, typically, a bath will not slow labor but allow for complete relaxation of the muscles between contractions.
The warmth and buoyancy of the water provides a measure of comfort throughout labor and birth. Slowly pouring water down the back or tummy is also helpful. Hydrotherapy and underwater birth is safe and reduces the need for pain medications while lowering your risk of a c-section due to the ability to move into and maintain open-pelvic positions for easier rotation and descent of the baby.
“A 2012 Cochrane review found no harm to the baby in 12 randomized controlled trials of water labor or birth involving 3,243 women, and less use of epidural anesthesia.”
The evidence shows that babies born in the water have similar health outcomes compared to babies born on land. The bottom line is that waterbirth is a reasonable option for low-risk birthing people.
An excerpt by Dr. Rebecca Dekker of Evidence Based Birth from her article titled Water Immersion During Labor for Pain Relief:
"The bottom line is that researchers have found that water immersion during labor poses no extra risks to the baby. They’ve overwhelmingly found that it lowers the need for pain medications and it makes people feel more satisfied with their pain relief. Hydrotherapy’s effectiveness on pain appears to be less effective than an epidural or spinal, but more effective than using IV opioid drugs. The good thing about water immersion during labor is that there doesn’t seem to be any side effects. Also, evidence shows that water immersion during labor increases people’s satisfaction with their childbirth and their sense of privacy and comfort. Mothers who labor and give birth in water tend to remember their experiences as being more positive and less painful." Read full article here.
We encourage you to explore for yourself all that underwater birth can offer you. Seek out medical facilities and care providers offering inflatable tubs or birth pools for labor and delivery (not just water "labor" or immersion). For further reading on water birth, checkout NPR's Shots article from March 2014.
How To Avoid a C-section Without Changing Hospitals For Less Than The Cost of a Latte A Day
Get dependable support for less than $5 per day of your pregnancy. Think about that. Then think about the cost of a c-section and an extended hospital stay. Hiring an experienced doula who works well with your care providers WILL SAVE YOU MONEY.
Do you know how to avoid the primary c-section? Hire a doula.
The American College of Obstetricians and Gynecologists (ACOG) backs this claim. An excerpt from their website:
"Today, approximately 60% of all cesarean births are primary cesareans. Although cesarean birth can be life-saving for the baby and/or the mother, the rapid increase in cesarean birth rates raises significant concern that cesarean delivery is overused without clear evidence of improved maternal or newborn outcomes."
Read ACOG's full article published March 2014: Safe Prevention of the Primary Cesarean Delivery, which discusses ways to decrease cesarean deliveries, including:
Allowing prolonged latent (early) phase labor.
Considering cervical dilation of 6 cm (instead of 4 cm) as the start of active phase labor.
Allowing more time for labor to progress in the active phase.
Allowing women to push for at least two hours if they have delivered before, three hours if it’s their first delivery, and even longer in some situations, for example, with an epidural.
Using techniques to assist with vaginal delivery, which is the preferred method when possible. This may include the use of forceps, for example.
Encouraging patients to avoid excessive weight gain during pregnancy.
One of the main points is to use continuous labor and delivery support:
"Published data indicate that one of the most effective tools to improve labor and delivery outcomes is the continuous presence of support personnel, such as a doula. A Cochrane meta-analysis of 12 trials and more than 15,000 women demonstrated that the presence of continuous one-on-one support during labor and delivery was associated with improved patient satisfaction and a statistically significant reduction in the rate of cesarean delivery (111). Given that there are no associated measurable harms, this resource is probably underutilized."
“Approximately 60% of all cesarean births are primary cesareans.”
At the hospital, laboring families aren't truly supported during childbirth unless they have a doula present. Care providers are quite busy and frequently enter and exit the room leaving you unattended while they are busy with other patients. Our birth doulas stay by your side and provide support when you need it most!
Still wonder if doula support is necessary? Research your hospital's c-section rate - many metro hospitals are WELL ABOVE the national average of 32.2%. Afterwards, watch The Business of Being Born, a documentary "eye-opener" about birth in America.
Simply put, our team helps you obtain your true childbirth options so you can have a great labor and birth experience.
For less money than you'd spend on a latte a day, you can hire an experienced labor doula.
Get dependable support for less than $5 per day of your pregnancy. Think about that. Then think about the cost of a c-section and an extended hospital stay. Hiring an experienced doula who works well with your care providers WILL SAVE YOU MONEY.
Many of our clients use their HSA/FSA debit cards to pay for childbirth services such as classes and doula support. Our agency includes our NPI number and taxonomy code on our order confirmations so you may attempt reimbursement from your insurance company or HSA/FSA accounts.
You should also note that we offer eGiftCards. If you receive a gift card after to you after you've paid, you'll be refunded the amount to the credit card used to reserve services through our website.
“For less money than you’d spend on a latte a day, you can hire help from an experienced labor doula.”
You'll remember your birthing experience forever. I wish you and your family a healthy and happy birthday.
Be well,
Cynthya
Click to visit http://www.lamaze.org/p/cm/ld/fid=160
Reference: Safe Prevention of the Primary Cesarean Delivery http://www.acog.org/Resources-And-Publications/Obstetric-Care-Consensus-Series/Safe-Prevention-of-the-Primary-Cesarean-Delivery
Lamaze Leads The Way: The Trusted Source of Childbirth Education
It is definitely advantageous for you to take a childbirth class but even more so to take a class taught by someone who has a lot of real-world knowledge and experience such as a Labor & Delivery nurse from the busiest hospital in the US.
by Lauren King, RN, Certified Lamaze Educator and DONA Birth Doula
For 55 years, Lamaze International has been the leading provider of evidence-based education programs that prepare childbirth educators to teach with skill and confidence. The Lamaze childbirth education certification is the only childbirth educator program that has passed rigorous standards set by the National Commission for Certifying Agencies (NCCA). The Lamaze certification program has been designed to meet the highest professional standards, with quality education offerings that help candidates develop as skilled, trusted LCCE educators.
I worked a labor and delivery nurse for 6 years before becoming a childbirth educator and doula. However, that alone didn’t make me a professional educator. In order to become certified through Lamaze as a Lamaze Certified Childbirth Educator (LCCE), I had to first attend a 2-day seminar. The seminars are not cheap, and they’re usually not nearby – making them even more of an investment. I drove to Raleigh, NC and stayed in a hotel for 3 nights to attend the seminar that led me on the path of certification.
In my seminar were people from all walks of life, but I was (surprisingly!) the only nurse! I couldn’t believe it. All these other people who had NO prior medical knowledge – very limited history on anatomy, maybe no formal knowledge of physiology, and most people in the class had extremely limited knowledge on labor and birth. My advantage to having medical experience was further made clear when we did a “medical lingo” activity. Do you know a “ctx” is? How about a toco? Do you know what pit stands for? (Contraction(s), uterine monitor and Pitocin.) So, yes, it is definitely advantageous for you to take a childbirth class, but even more so to take a class from someone who has a lot of real-world knowledge and experience.
“I chose Lamaze because around the world, it is a well-known and trusted name in childbirth for the past 55 years.”
After my seminar was complete, I had a mentor observe me teach a class. Afterward, I was permitted to sign up for the certification exam. It is only offered twice a year and has around 150 questions. I sat in a little closet (literally) with a desk, a chair, and the computer in front of me. Talk about stressful! A few weeks later, I was notified that I had passed the test, and I was officially a Lamaze Certified Childbirth Educator.
Now, to maintain my certification, every 3 years, I must submit 25 hours of approved continuing education, as well as make another monetary investment. (This is on top of the 30 hours and monetary investment I have to submit every two years to maintain my nursing license!) Lamaze does an awesome job of offering a lot of those hours through various seminars and workshops. The courses I take must relate to one of the seven Lamaze Childbirth Educator Competencies:
Competency 1: Promotes the childbearing experience as a normal, natural, and healthy process which profoundly affects women and their families.
Competency 2: Assists women and their families to discover and to use strategies to facilitate normal, natural, and healthy pregnancy, birth, breastfeeding, and early parenting.
Competency 3: Helps women and their families to understand how complications and interventions influence the normal course of pregnancy, birth, breastfeeding and early postpartum.
Competency 4: Provides information and support that encourages attachment between babies and their families.
Competency 5: Assists women and their families to make informed decisions for childbearing.
Competency 6: Acts as an advocate to promote, support, and protect natural, safe and healthy birth.
Competency 7: Designs, teaches, and evaluates a course in Lamaze preparation that increases a woman’s confidence and ability to give birth.
Don’t take childbirth education too lightly!
As your educator, I LOVE teaching you everything I possibly can about pregnancy and birth. I do it because it is my passion! I chose Lamaze because around the world, it is a well-known and trusted name in childbirth for the past 55 years. Lamaze International stays up-to-date on all the current research and recommendations, and I pass all of this on to my students.
Knowledge is power but only if you know how to apply it to your situation. Schedule a private childbirth lesson in your home to maximize your chances of a having a comfortable and relaxed birthday party.
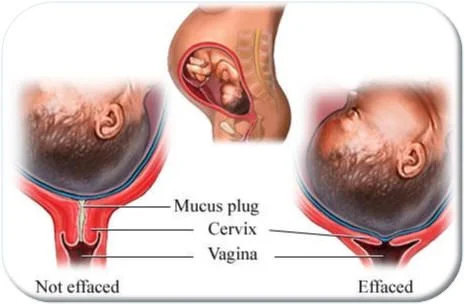
Vaginal Exams Don't Predict Labor
Clients often misinterpret the residual symptoms of a vaginal exam for signs of labor starting on its own.
Beware! Around your 39th week of pregnancy, your OB or midwife will offer or expect you to have a vaginal exam. You should know these exams do not determine when labor will begin but do introduce bacteria, may cause bleeding and cramping, and risk premature rupture of the membranes, which could force an induction if labor doesn't begin within 24 hours.
"Clients often misinterpret the residual symptoms of a vaginal exam for signs of labor starting on its own." - click to tweet!
Once a client called me in tears stating that during an exam at her week 41 appointment, her OB "stripped her membranes" without her permission "to get things going." Ouch!
Unless you are in labor or about to be induced, knowing your dilation or effacement is not helpful. Many clients experience the early stage of labor for days (even weeks) or are a few centimeters dilated without contractions and it doesn't amount to much. Bottom line is: it may hurt, cause issues, and isn't helpful so why endure this highly inaccurate assessment?
Labor is divided into four stages
No one can predict when your body will begin labor. As a reminder, the stages of labor and what to expect for each are below.
Stage ONE is further divided into three phases:
Phase I: Early labor also called the latent phase.
Phase II: Active labor (5cm or 6cm dilation to 8cm)
Phase III: Transition (8cm dilation to 10cm or "complete")
Stage TWO: also called the pushing stage.
Stage THREE: the birth of your placenta.
Stage FOUR: the hour after birth.
For an overview of labor and birth with suggestions for progress and comfort, keep this webpage linked from your phone. To limit the amount of interventions throughout labor and birth, review our 7 part series, How To Alleviate Fears and Manage Labor Pain. To help you find out if your care provider is practicing within the current guidelines, read ACOG’s Committee Opinion, and ask your doctor what you can expect in the possible scenarios and how they will support your goals for baby’s birthday.
Stay in the know
The Happiest Doulas maintains a Pinterest board, Labor & Birth Support; Tips from Doulas, Midwives, and Educators. Follow it for more labor and birth tips from trusted resources around the world.
Stay well,
Cynthya
Related articles:
Avoid Routine Medical Interventions
Episiotomy and C-section Rates
AROM: To Break or Not To Break2 More Reasons You Don’t Need an Induction
No two pregnancies are the same (even within the same body), no two labors are the same; there are so many factors that play into a pregnancy and her subsequent labor and birth.
by Lauren King, Registered Nurse, Certified Lamaze Educator, and DONA Labor Doula
What is the average size of a baby born in America? Would you guess 7 pounds? Maybe 7 and a half? Eight pounds. Eight pounds is the average size of babies born in America. That means some (lots!) of babies are bigger than that – and many babies are smaller than that. Genetics and mom’s lifestyle, among other things, play a huge role in how big you grow your babies. I’ve seen babies born vaginally that weighed over 10 pounds! I’ve heard stories of babies just as large born vaginally with no pain medication! It’s certainly not impossible. (Maybe not necessarily the most pleasant thought… but not impossible!) Do you know how much amniotic fluid is adding to your weight? Well, not much honestly, but if you’re around 34 weeks, you have now reached the peak amount of amniotic fluid at about 800 mL. From 34 weeks on, amniotic fluid levels will gradually decline. Read on to learn why this matters.
Some doctors suggest an induction for “big baby” because they believe it decreases the chance of a shoulder dystocia (difficulty delivering the shoulders) or the need for a cesarean due to the baby being too large to fit through the pelvis. However, research shows this is simply not true. The risk of shoulder dystocia is relatively small – and it’s impossible to predict who will have a shoulder dystocia. Furthermore, for a doctor to suggest a woman to induce for this reason, the doctor must assume the ultrasound is accurately assessing the size of the baby. Next time a late-pregnancy ultrasound is recommended to you to assess fetal size during your pregnancy, ask your doctor or the sonographer how accurate it is. If they tell you the baby “might” weigh about 8 pounds, please know they can be off by as much as 2 pounds either direction. There is a HUGE difference between a 6 pound baby, an 8 pound baby, and a 10 pound baby. I have seen elective c-sections performed on first-time mothers due to “possible macrosomia” (big baby), only to discover the baby weighed LESS than 8 pounds.
I often tell people that things in labor and delivery can be very dynamic. The more I think about it, the more I realize how true that statement is in so many ways. No two pregnancies are the same (even within the same body), no two labors are the same; there are so many factors that play into a pregnancy and her subsequent labor and birth. Another dynamic aspect of pregnancy? Amniotic fluid. As I mentioned above, the amount of amniotic fluid peaks at about 34 weeks, reaching around 800 mL, and gradually declines to around 600 mL by 40 weeks. However, there are many factors that can play into these numbers. The baby, the mother, and the sonographer measuring the amniotic fluid can all affect the actual or perceived level of fluid.
The baby constantly circulates the fluid by inhaling it, swallowing it, and then releasing it through the urinary tract. Near term, the baby swallows more and urinates less often, thereby holding more fluid at any given time. Other baby-driven factors include: post-term (past 42-weeks), birth defect, or problems with the kidneys or urinary tract.
If you are dehydrated, such as in the coming summer months especially, if your water is broken, or if the placenta is no longer functioning properly, you may be diagnosed with low amniotic fluid. Some things you may try to increase amniotic fluid levels include drinking more water (at least 2-3 liters a day) and laying on your left side during an ultrasound when measuring fluid levels. Other factors that can play into an inaccurate reading include too much pressure on the ultrasound transducer, floating particles in the fluid, and an obese mother. Yes, “low amniotic fluid” could be a sign of a health issue and can be a medical reason for induction, but ask your doctor what their specific concern is before agreeing to induction simply for “low amniotic fluid.” Furthermore, you may wish to have a reevaluation in a couple days. Drink lots and lots of water, and when you return for another ultrasound (hopefully by the same sonographer!), if the fluid level is still low, or has decreased further, then you may wish to discuss the next step with your provider. If it has increased, then you might have saved yourself from an unnecessary induction! For a brand new diagnosis of “low fluid” without any other known cause, you may be better off to wait.
"What I have heard, and what I suspect it ultimately boils down to, is for one thing, doctors are human." - tweet this!
So, knowing all of this, why do doctors recommend things that are not backed by research or ACOG? My honest answer is: I don’t know. What I have heard, and what I suspect it ultimately boils down to, is that for one thing, doctors are human. Meaning: doctors want convenience and easy and predictable and good ratings. What? Good ratings? Exactly. Doctors and hospitals have a business to run. They have to keep their patients happy to keep them coming back for subsequent care! And businesses are consumer-driven. How many times have you heard that you can’t treat a viral infection with antibiotics? And yet, when a patient goes into a doctor’s office, demanding something to be done about their illness, they just might walk out with an antibiotic prescription in hand. Same thing with inductions. When a patient begs, pleads, whines, and complains about all the aches and pains, and difficulties of pregnancy, their doctor wants to appease them. No, not all doctors act this way, but the ones that do are the ones contributing to the problem and making it “okay” for other doctors to do the same. Although, I have to say – it’s not ALL the doctors’ faults. We, as women, as mothers, as consumers are just as much to blame. If I walk into my doctor’s office, demanding an induction – all the while, knowing all the risks of doing such – my doctor doesn’t want to lose me as a customer, so he agrees.
You Have More Power Than You Know
On the flip side, if more women – more consumers – are asking their doctors to allow their bodies to go into labor naturally, they will stop suggesting and allowing for non-medical inductions. If more women are getting educated on their options and on the pros and cons of such procedures, and refusing inductions for the sake of convenience, doctors will follow suit. Ultimately, they want to make their customers happy.
For more information on inductions, please visit MedLine Plus, American Pregnancy Association, and the Adventures of a Labor Nurse.
"Amniotic fluid peaks at 34 weeks, reaching around 800 mL, and gradually declines to around 600 mL by 40 weeks." - tweet this!
Related articles:
Knowing Your Options Is Vital To Your Labor And Birth
How To Avoid a C-section Without Changing Hospitals
6 Comfort Tips For NOT Breastfeeding
So You Need An Induction, Eh?