"Cynthya was our doula for the birth of our third child in April 2016. As this was my third birth, and I had been attended to by a doula at the first two, I knew that finding the right doula was crucial to a successful and satisfying birth." - Winter Wheeler-Young
6 Ways to Survive a Colicky Baby
"Was I enjoying my sweet, new baby? No. I wanted my old life back. I wanted to run away. More than anything, I wanted to sleep for days."
I remember running into an acquaintance a couple of months after my son was born. “Are you enjoying that sweet, new baby?” she asked. I stared blankly. The weight of exhaustion made it impossible to fake my enthusiasm, so I gave a long, deep sigh. The correct answer was obvious. Doesn't every new mom enjoy their precious new baby? The truth was that I wasn't.
He nursed constantly, refused to take a bottle, would only sleep on top of me or in my arms, screamed every time he was in his car seat. Starting at around 4 pm, every single day, he would become inconsolable and cry. A LOT. I swaddled, nursed, rocked, walked, shushed, begged, and cried with him for hours. This is how I spent most of my afternoons. Was I enjoying my sweet, new baby? No. I wanted my old life back. I wanted to run away. More than anything, I wanted to sleep for days.
Having a high needs or colicky infant feels relentless. Those afternoons stretched before me, and I knew that, unlike what everyone said, this was not going to pass. Time had stopped, and this would go on for the rest of my life. I was Sisyphus, condemned to push a boulder up a hill, with a crying infant strapped to my back.
“I was Sisyphus, condemned to push a boulder up a hill, with a crying infant strapped to my back.”
Everyone was right, though. My son is almost 2 now. He is smart, funny, healthy, and delightful. Here are some tips and techniques I learned along the way, and also some things that I will do differently if I have another child:
Rest when you can. I often found it difficult to sleep during the day, but just closing my eyes in a quiet, dark room helped me recharge. And don't worry if you can't get to sleep. It will get better, and you will sleep again. Being anxious about not sleeping only makes it less likely that you will sleep.
Take a "Mailbox Moment." If you are feeling overwhelmed, put your baby down in safe place, and walk away. Go outside, take deep breaths. I felt guilty when I did this because I wanted to be able to fix it, and I thought a good mother should know how to do that. Now I know that a good mother knows she needs to take care of herself along the way.
Ask for help, and take it when people offer! I found it helpful when my husband would take the baby for a walk. A quiet house and the bliss of aloneness were so healing for me.
Read the Happiest Baby on the Block, and use the “5 S System.” At the time, I had not read the book, but my son's pediatrician recommended the techniques in it. Swaddling and making a loud shushing sound with movement were particularly helpful. If you have a colicky baby, you should know that, while these techniques do help to take the sting out, they may not be the magic solution you're needing. They certainly help, but only time will definitely end the problem.
Hire a postpartum doula. When I became a mom, I didn't have much experience with newborns. While much of the care is instinctual and learned along the way, having a trained and experienced professional would have been so helpful in the transition. A postpartum doula will help the new family by providing emotional support and guidance in newborn care, while helping you get your bearings as a new mom and family.
The most important thing to remember is that it is just a season. It isn't forever. Even though it feels like it is. It really will get better. Now, I look at my wonderful two year old son, and those sleep deprived, colicky days feel like a lifetime ago. In many ways, they were a lifetime ago because I'm not the woman I used to be.
Colic does end. You can survive it, and come out better and stronger on the other side of it. Motherhood is a journey, and journeys aren't always easy. But they are worth it.
How To Stop a Baby's Crying and Other Must-Know Tricks
This method saves the sanity of new parents and provides REAL tools to comfort baby.
Stop a baby's crying and ease colic instantly with Dr. Harvey Karp's internationally known "prescription". This method saves the sanity of new parents and provides REAL tools to comfort baby. Watch the video below, memorize the fabulous Cuddle Cure and Calming Reflex, and use the method to enjoy long periods of sleep.
For more in-depth guidance, look into a private, in-home lesson with us. A consult includes newborn care information such as diapering, co-sleeping safety, SIDS awareness, and sleep scheduling, as well as the Cuddle Cure for ending colic.
How Does a Braxton-Hicks Contraction Feel?
What does a Braxton-Hicks contraction feel like?
How to Make Healthy and Safe Decisions During Pregnancy and Parenting
This new resource is great for expecting parents and their partners to help them keep track of important events, questions to ask, and even has a contraction timer.
Lamaze launched its first-ever mobile application for parents, Pregnancy to Parenting. This unique app is complete with evidence-based weekly development updates, daily tips and helpful tools developed by Lamaze Certified Childbirth Educators. This new resource is great for expecting parents and their partners to help them keep track of important events, questions to ask, and even has a contraction timer. The best part is that it is free to download - try it today.
Lamaze Leads The Way: The Trusted Source of Childbirth Education
It is definitely advantageous for you to take a childbirth class but even more so to take a class taught by someone who has a lot of real-world knowledge and experience such as a Labor & Delivery nurse from the busiest hospital in the US.
by Lauren King, RN, Certified Lamaze Educator and DONA Birth Doula
For 55 years, Lamaze International has been the leading provider of evidence-based education programs that prepare childbirth educators to teach with skill and confidence. The Lamaze childbirth education certification is the only childbirth educator program that has passed rigorous standards set by the National Commission for Certifying Agencies (NCCA). The Lamaze certification program has been designed to meet the highest professional standards, with quality education offerings that help candidates develop as skilled, trusted LCCE educators.
I worked a labor and delivery nurse for 6 years before becoming a childbirth educator and doula. However, that alone didn’t make me a professional educator. In order to become certified through Lamaze as a Lamaze Certified Childbirth Educator (LCCE), I had to first attend a 2-day seminar. The seminars are not cheap, and they’re usually not nearby – making them even more of an investment. I drove to Raleigh, NC and stayed in a hotel for 3 nights to attend the seminar that led me on the path of certification.
In my seminar were people from all walks of life, but I was (surprisingly!) the only nurse! I couldn’t believe it. All these other people who had NO prior medical knowledge – very limited history on anatomy, maybe no formal knowledge of physiology, and most people in the class had extremely limited knowledge on labor and birth. My advantage to having medical experience was further made clear when we did a “medical lingo” activity. Do you know a “ctx” is? How about a toco? Do you know what pit stands for? (Contraction(s), uterine monitor and Pitocin.) So, yes, it is definitely advantageous for you to take a childbirth class, but even more so to take a class from someone who has a lot of real-world knowledge and experience.
“I chose Lamaze because around the world, it is a well-known and trusted name in childbirth for the past 55 years.”
After my seminar was complete, I had a mentor observe me teach a class. Afterward, I was permitted to sign up for the certification exam. It is only offered twice a year and has around 150 questions. I sat in a little closet (literally) with a desk, a chair, and the computer in front of me. Talk about stressful! A few weeks later, I was notified that I had passed the test, and I was officially a Lamaze Certified Childbirth Educator.
Now, to maintain my certification, every 3 years, I must submit 25 hours of approved continuing education, as well as make another monetary investment. (This is on top of the 30 hours and monetary investment I have to submit every two years to maintain my nursing license!) Lamaze does an awesome job of offering a lot of those hours through various seminars and workshops. The courses I take must relate to one of the seven Lamaze Childbirth Educator Competencies:
Competency 1: Promotes the childbearing experience as a normal, natural, and healthy process which profoundly affects women and their families.
Competency 2: Assists women and their families to discover and to use strategies to facilitate normal, natural, and healthy pregnancy, birth, breastfeeding, and early parenting.
Competency 3: Helps women and their families to understand how complications and interventions influence the normal course of pregnancy, birth, breastfeeding and early postpartum.
Competency 4: Provides information and support that encourages attachment between babies and their families.
Competency 5: Assists women and their families to make informed decisions for childbearing.
Competency 6: Acts as an advocate to promote, support, and protect natural, safe and healthy birth.
Competency 7: Designs, teaches, and evaluates a course in Lamaze preparation that increases a woman’s confidence and ability to give birth.
Don’t take childbirth education too lightly!
As your educator, I LOVE teaching you everything I possibly can about pregnancy and birth. I do it because it is my passion! I chose Lamaze because around the world, it is a well-known and trusted name in childbirth for the past 55 years. Lamaze International stays up-to-date on all the current research and recommendations, and I pass all of this on to my students.
Knowledge is power but only if you know how to apply it to your situation. Schedule a private childbirth lesson in your home to maximize your chances of a having a comfortable and relaxed birthday party.
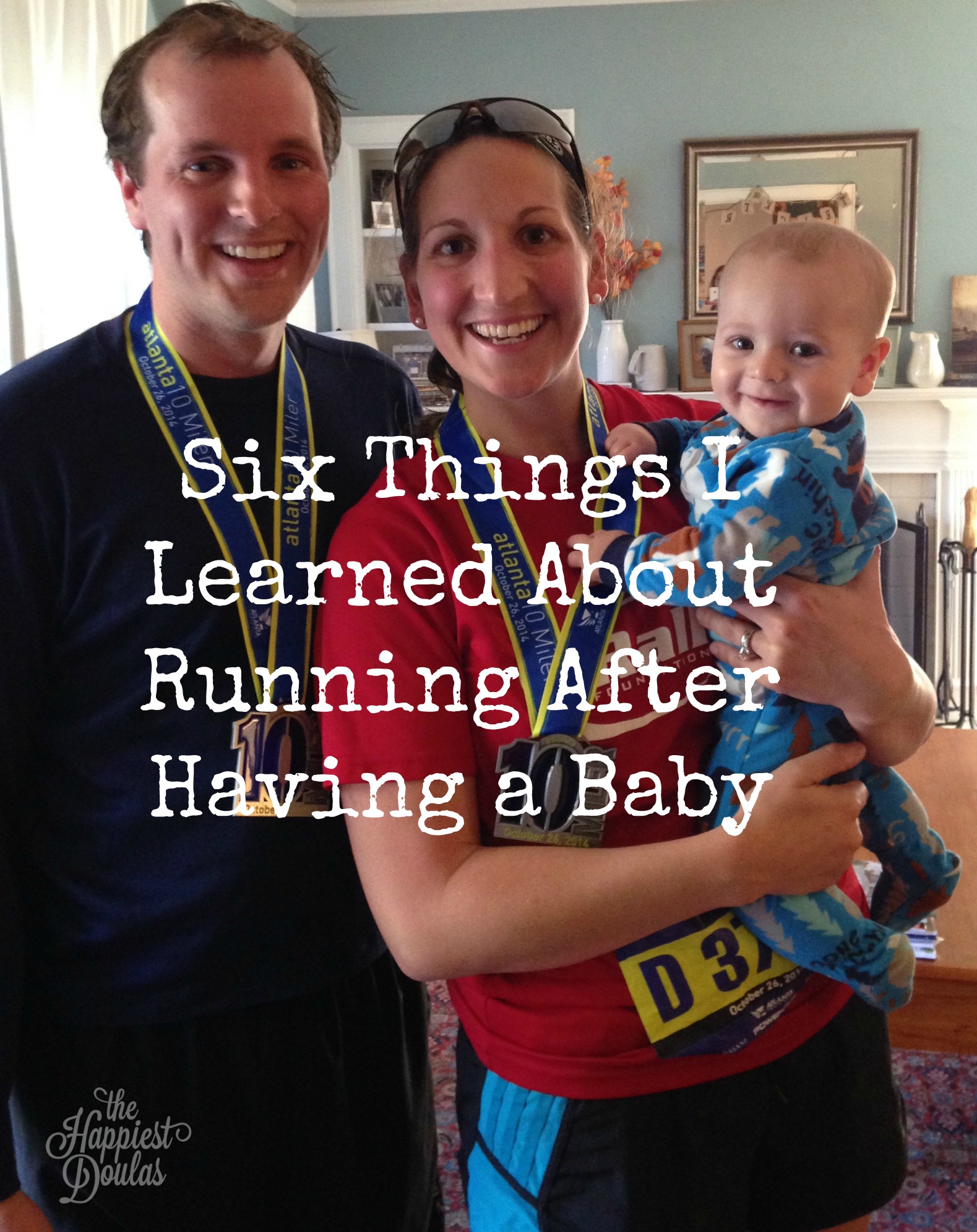
What Every Female Runner Should Know Postpartum
Whether you were a running before you had a baby or not, running is an attractive exercise option for moms. It is much easier to lace up your shoes run out the door than going to a gym.
by Dr. Kate Mihevc Edwards
I am a mom, a runner and a triathlete. I have the benefit of being a physical therapist (PT) that specializes in treating runners and triathletes and I work in an office with two knowledgeable pelvic health PTs. My son just turned one and I, too, am still re-learning my body. Over and over I have heard friends and patients talk about wearing a pad when they run because of leaking or getting a stress fracture while they are breastfeeding. I hear about how exhausted they are how hard they are working to get their abs back to pre-pregnancy form.
In 2013, Running USA reported that female runners are at an all time high with 8.6 million female race finishers nationwide and females accounting for 56% of all race finishers. With over 4 million babies born in the U.S. each year, I wonder how many of these women have had babies and how many have had questions about how to return to running after their babies.
Whether you were a running before you had a baby or not, running is an attractive exercise option for moms. It is much easier to lace up your shoes run out the door than going to a gym. For me, running is a gift; it allows me a few minutes of alone time as well as some needed freedom by taking my son with me on the run. A recent study even found that women who ran while breastfeeding had a significantly lower incidence of postpartum depression.*
It is difficult to find information or resources for women when we return to running or start running postpartum. Most women have no idea where to start, what to expect, how their body should feel and what is/isn’t normal. By addressing these issues and educating ourselves and others about how our bodies change during the months after childbirth, we can significantly reduce the potential for injury.
Things I’ve learned along my journey back to running
Don’t start running too soon! Believe me I wanted to run as soon as possible, I bargained with myself nearly every day, but in the end I took the advice of one of my colleagues and waited 8 weeks. I was very glad I did. Friends of mine that did not wait long enough have had a more difficult time finding their stride and a few have even been injured. A recent article reported one quarter of the women in their study resumed running two or fewer weeks postpartum.* The body is undergoing rapid, tremendous change during the first 2-6 months postpartum. Starting too soon may put you at risk for injury.
I recommend you consult 2 professionals before returning to running:
Your Physician. Your Ob/Gyn will be able to tell you whether your body is healing appropriately and whether it is safe to return to running. Women who deliver vaginally may be able to return to running sooner than those who undergo a Cesarian Section.
A Pelvic Health Physical Therapist. I did this and suggest all of my friends to do this too. Being a PT I knew how important it was and wanted to go right away, but was told to wait until approximately 6-8 weeks postpartum. Even though I am a PT and know my body very well I still learned so much. Your therapist will be able to assess how your muscles are functioning and can guide you on how to return to exercise safely. The pelvic floor is the “floor of your core.” By keeping this muscle strong and functioning well, it will help you stay injury free. If it is not working then it will set you up for issues later on.
Returning to running after a baby is hard.
You are exhausted, you are heavier, and your breasts hurt. I had to run with two sports bras just to be comfortable. No matter what kind of runner you were before your munchkin was born take it easy on yourself. Your body did an amazing thing; give it a break. You will get there.
I have completed several triathlons, 14 marathons including 3 Boston marathons under my belt. When I started running again I was so excited and defeated all at once. I was running again, yet I ran 4:00 minutes/mile slower than usual, for a long time. Almost a year later, and still breastfeeding, my feet are beginning to move quickly again. It is okay to pace yourself, go slow and work your way back to your pre-pregnancy PR. Enjoy the time you have to exercise and all the benefit it brings; the speed will come.
“Leaking is common, but NOT normal.”
This is one of my favorite quotes from a colleague of mine, Blair Green, PT who specializes in treating woman and the pelvic floor. When I went to my postpartum yoga class everyone was talking about how they would pee accidentally. I couldn’t believe how common and accepted this was. Of course I was the obnoxious one screaming NO! It is not okay! I gave out a lot of Blair’s business cards and got a lot of words of thanks later.
If you are leaking when you cough, sneeze, jump or run make an appointment with a local pelvic health PT. There is no reason you should just deal with this. A good pelvic health PT can screen your musculoskeletal system and identify areas of impairment in muscle length, strength and function that may be holding you back from full return to running.
You are at higher risk for stress fractures when you are breastfeeding.
I tell you this so that you are aware. It makes sense - you are producing food for another human. Your body will choose to make milk over maintaining your bone health. You need to make sure you are getting enough calories and not running too much too soon.
It is far worse to get a stress fracture and not be able to run than it is to ease into running and stay healthy. Believe me you do not want to be in a walking boot trying to chase a toddler or carrying a baby in a car seat.
Have you ever heard of a diastasis recti?
Essentially it is a split in the abdominal wall muscles. Some women have them and do not realize it and for others it is very noticeable. If you feel a vertical gap between your abs at, above, or below your belly button, especially when engaging your abdominals it is possible you have one. There have been studies that link having a diastasis to stress incontinence in women even years after having their babies.**
Doing sit-ups and a lot of abdominal exercises can make this condition worse, not better. Again this is another issue that can be addressed by a PT and possibly a knowledgeable Pilates instructor. If you choose to try and address this with Pilates it is important that your instructor truly understands and has experience working with postpartum women with diastasis. It would be ideal that your PT clear you to participate in Pilates first.
Maintaining good running form while pushing a stroller is extremely difficult.
I help people improve their running form all day long, everyday and it is still difficult for me to push the stroller with good form. Ideally, you want to do your best to maintain a fairly normal stride and good posture.
Try not to lean forward from the hips when pushing the stroller in front of you. I notice this happens more when people are going uphill. Think about keeping your rib cage stacked over your pelvis and breathing for optimal stability. If you are pushing the stroller with two hands hold onto the handle on the outside edge in order to keep you thumbs towards the sky and elbows towards the ground. If you are pushing with one arm and swinging the other be sure to switch back and forth between sides periodically.
The bottom line is in order to carry, deliver and nourish a child, your body has to change and adapt. These changes can affect your running and put you at risk for injury but they don’t have to if you are aware of the common issues postpartum women face. So next time you hear your friend talking about peeing when they run or her say she is still breastfeeding but wants to get back to her 30-40 miles/week ASAP talk about it- the more we talk about the common issues women have the more “normal” it is to address them. My goal is always to keep runners running. Be smart and utilize your resources around you. Running has been shown to improve mood, cognition and has extensive health benefits, so keep running ladies! I hope to see you out there looking strong and kicking butt as you push your BOB or double BOB up those hills!
References:
*Tenforde, A.S., et al (2015) Running Habits of Competitive Runners During Pregnancy and Breastfeeding. Sports Health a Multidisciplinary Approach, 7(2) 172-176.
**Spitznagle TM, Leong FC, van Dillen LR 2007 Prevalence of diastasis recti abdominis in a urogynecological patient population. Int Urogynecology
Dr. Edwards is a Physical Therapist that specializes in treating runners and triathletes. She is the co-founder of Precision Performance Consulting LLC where she performs comprehensive running analysis for runners of all ages and abilities. She is an adjunct professor in the Emory University Physical Therapy School of Medicine and works as a Physical Therapist at Back 2 Motion Physical Therapy in Atlanta, GA.
4 Things To Do Now For a Healthier Postpartum
Whether it’s your first or fifth baby, here are four things you can do NOW to prep for a healthy jumpstart postpartum.
by guest blogger, Amanda Bifulco, health coach, yogi and mom (also a client of The Happiest Doulas)
I’ve found that clients struggle the most with staying on top with health goals when they aren’t prepared. Start preparing now for the healthiest postpartum you can create. Your body, and your baby, will thank you. Whether it’s your first or fifth baby, here are four things you can do NOW to prepare for a healthy postpartum jumpstart.
1. Cook & Store
Before the birth of my son, I stocked my freezer with meals that would be easy to heat up and eat. I recommend, clients make sure there are plenty of healthy options that don’t require a lot of work to prepare. I knew my husband and I would both be tired and could quickly take the easy way out (pizza or other delivered fast food) if not prepared. I exclusively breast feed, and these didn’t seem to impact little man’s tummy, but it’s easy to scale back on the flavor (less salsa, less tomato, less Balsamic vinegar) if you think they’re contributing to an upset tummy for your baby.
2. Have a Fitness Plan
You don’t know how your labor and recovery is going to go. Every woman is different and every labor is different though everybody needs some time to recover. Physical movement can be part of that recovery and ultimately help you feel better faster. Have a fitness plan and have a goal in mind.
““Even if your labor and delivery go as perfectly as planned, these four suggestions can help you have a healthier postpartum and settle in at home a little bit easier.”
My plan was to get back to walking the dog as quickly as possible. Within days of getting home, even though I was exhausted, I put on some sneakers and took the dog for a walk up and down the block, while family stayed home with baby. I didn’t go far or fast, but I can’t tell you how AMAZING the fresh air and sunshine felt. It was February and it was cold out, but it felt glorious to be outside. When I came back I felt like a new person. True story. After that, my goals were to start gentle yoga and, once cleared by my doctor, get back to the gym.
3. Grocery Shopping
As many do, I make a grocery list when I go to the store. As we got closer to our due date, I made a list of essentials and non-essentials that my husband could pick up when he was on his way home or out and about. For example, we can never have too much almond milk or eggs. Seriously. We go through that stuff like water. Plus, if we DO end up with some extra, I make almond milk ice cubes, a quiche for dinner, or egg muffins and freeze them. Anyways, I digress…have a list of essentials that ANYONE can pick up for you. If a friend is stopping by to visit you and the baby and asks if you need anything: essentials.
Family member willing to run to the store, what do you need: essentials. Going to the doctor and significant other will run into the store: essentials. You THINK you’ll remember what these essentials are but you probably won’t. And someone will offer and you won’t be able to come up with anything. WRITE THINGS DOWN.
4. Vitamins
High five for taking pre-natal vitamins throughout your pregnancy, but don’t stop now! Let’s review: you just birthed a BABY. Your body is recovering from delivery. You’re going to lose sleep. You’re body still needs essential vitamins and nutrients supplemental to your diet. And I didn’t even mention breastfeeding, if you plan to. Have a multivitamin ready to start taking immediately. I kept on taking my prenatal vitamins until I ran out and then switched to a high quality multi-vitamin.
Even if your labor and delivery goes perfectly as planned, these four suggestions can help you have a healthier postpartum and settle in at home a little bit easier.
About the author:
Amanda Bifulco currently lives in Virginia with her husband, dog and son. While not busy being a mom, coaching or pursuing her own fitness goals, she’s blogging tips and tricks to help others reach their weight loss or fitness goals. Find out more about Amanda here or connect with her on Facebook or via Twitter and IG @AmandaJoyFit.
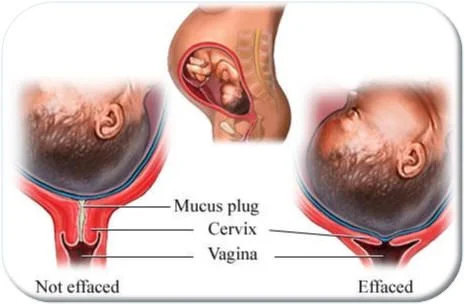
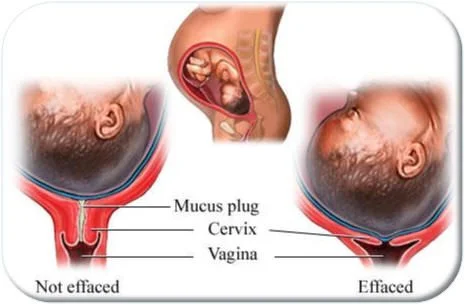
Vaginal Exams Don't Predict Labor
Clients often misinterpret the residual symptoms of a vaginal exam for signs of labor starting on its own.
Beware! Around your 39th week of pregnancy, your OB or midwife will offer or expect you to have a vaginal exam. You should know these exams do not determine when labor will begin but do introduce bacteria, may cause bleeding and cramping, and risk premature rupture of the membranes, which could force an induction if labor doesn't begin within 24 hours.
"Clients often misinterpret the residual symptoms of a vaginal exam for signs of labor starting on its own." - click to tweet!
Once a client called me in tears stating that during an exam at her week 41 appointment, her OB "stripped her membranes" without her permission "to get things going." Ouch!
Unless you are in labor or about to be induced, knowing your dilation or effacement is not helpful. Many clients experience the early stage of labor for days (even weeks) or are a few centimeters dilated without contractions and it doesn't amount to much. Bottom line is: it may hurt, cause issues, and isn't helpful so why endure this highly inaccurate assessment?
Labor is divided into four stages
No one can predict when your body will begin labor. As a reminder, the stages of labor and what to expect for each are below.
Stage ONE is further divided into three phases:
Phase I: Early labor also called the latent phase.
Phase II: Active labor (5cm or 6cm dilation to 8cm)
Phase III: Transition (8cm dilation to 10cm or "complete")
Stage TWO: also called the pushing stage.
Stage THREE: the birth of your placenta.
Stage FOUR: the hour after birth.
For an overview of labor and birth with suggestions for progress and comfort, keep this webpage linked from your phone. To limit the amount of interventions throughout labor and birth, review our 7 part series, How To Alleviate Fears and Manage Labor Pain. To help you find out if your care provider is practicing within the current guidelines, read ACOG’s Committee Opinion, and ask your doctor what you can expect in the possible scenarios and how they will support your goals for baby’s birthday.
Stay in the know
The Happiest Doulas maintains a Pinterest board, Labor & Birth Support; Tips from Doulas, Midwives, and Educators. Follow it for more labor and birth tips from trusted resources around the world.
Stay well,
Cynthya
Related articles:
Avoid Routine Medical Interventions
Episiotomy and C-section Rates
AROM: To Break or Not To Break2 More Reasons You Don’t Need an Induction
No two pregnancies are the same (even within the same body), no two labors are the same; there are so many factors that play into a pregnancy and her subsequent labor and birth.
by Lauren King, Registered Nurse, Certified Lamaze Educator, and DONA Labor Doula
What is the average size of a baby born in America? Would you guess 7 pounds? Maybe 7 and a half? Eight pounds. Eight pounds is the average size of babies born in America. That means some (lots!) of babies are bigger than that – and many babies are smaller than that. Genetics and mom’s lifestyle, among other things, play a huge role in how big you grow your babies. I’ve seen babies born vaginally that weighed over 10 pounds! I’ve heard stories of babies just as large born vaginally with no pain medication! It’s certainly not impossible. (Maybe not necessarily the most pleasant thought… but not impossible!) Do you know how much amniotic fluid is adding to your weight? Well, not much honestly, but if you’re around 34 weeks, you have now reached the peak amount of amniotic fluid at about 800 mL. From 34 weeks on, amniotic fluid levels will gradually decline. Read on to learn why this matters.
Some doctors suggest an induction for “big baby” because they believe it decreases the chance of a shoulder dystocia (difficulty delivering the shoulders) or the need for a cesarean due to the baby being too large to fit through the pelvis. However, research shows this is simply not true. The risk of shoulder dystocia is relatively small – and it’s impossible to predict who will have a shoulder dystocia. Furthermore, for a doctor to suggest a woman to induce for this reason, the doctor must assume the ultrasound is accurately assessing the size of the baby. Next time a late-pregnancy ultrasound is recommended to you to assess fetal size during your pregnancy, ask your doctor or the sonographer how accurate it is. If they tell you the baby “might” weigh about 8 pounds, please know they can be off by as much as 2 pounds either direction. There is a HUGE difference between a 6 pound baby, an 8 pound baby, and a 10 pound baby. I have seen elective c-sections performed on first-time mothers due to “possible macrosomia” (big baby), only to discover the baby weighed LESS than 8 pounds.
I often tell people that things in labor and delivery can be very dynamic. The more I think about it, the more I realize how true that statement is in so many ways. No two pregnancies are the same (even within the same body), no two labors are the same; there are so many factors that play into a pregnancy and her subsequent labor and birth. Another dynamic aspect of pregnancy? Amniotic fluid. As I mentioned above, the amount of amniotic fluid peaks at about 34 weeks, reaching around 800 mL, and gradually declines to around 600 mL by 40 weeks. However, there are many factors that can play into these numbers. The baby, the mother, and the sonographer measuring the amniotic fluid can all affect the actual or perceived level of fluid.
The baby constantly circulates the fluid by inhaling it, swallowing it, and then releasing it through the urinary tract. Near term, the baby swallows more and urinates less often, thereby holding more fluid at any given time. Other baby-driven factors include: post-term (past 42-weeks), birth defect, or problems with the kidneys or urinary tract.
If you are dehydrated, such as in the coming summer months especially, if your water is broken, or if the placenta is no longer functioning properly, you may be diagnosed with low amniotic fluid. Some things you may try to increase amniotic fluid levels include drinking more water (at least 2-3 liters a day) and laying on your left side during an ultrasound when measuring fluid levels. Other factors that can play into an inaccurate reading include too much pressure on the ultrasound transducer, floating particles in the fluid, and an obese mother. Yes, “low amniotic fluid” could be a sign of a health issue and can be a medical reason for induction, but ask your doctor what their specific concern is before agreeing to induction simply for “low amniotic fluid.” Furthermore, you may wish to have a reevaluation in a couple days. Drink lots and lots of water, and when you return for another ultrasound (hopefully by the same sonographer!), if the fluid level is still low, or has decreased further, then you may wish to discuss the next step with your provider. If it has increased, then you might have saved yourself from an unnecessary induction! For a brand new diagnosis of “low fluid” without any other known cause, you may be better off to wait.
"What I have heard, and what I suspect it ultimately boils down to, is for one thing, doctors are human." - tweet this!
So, knowing all of this, why do doctors recommend things that are not backed by research or ACOG? My honest answer is: I don’t know. What I have heard, and what I suspect it ultimately boils down to, is that for one thing, doctors are human. Meaning: doctors want convenience and easy and predictable and good ratings. What? Good ratings? Exactly. Doctors and hospitals have a business to run. They have to keep their patients happy to keep them coming back for subsequent care! And businesses are consumer-driven. How many times have you heard that you can’t treat a viral infection with antibiotics? And yet, when a patient goes into a doctor’s office, demanding something to be done about their illness, they just might walk out with an antibiotic prescription in hand. Same thing with inductions. When a patient begs, pleads, whines, and complains about all the aches and pains, and difficulties of pregnancy, their doctor wants to appease them. No, not all doctors act this way, but the ones that do are the ones contributing to the problem and making it “okay” for other doctors to do the same. Although, I have to say – it’s not ALL the doctors’ faults. We, as women, as mothers, as consumers are just as much to blame. If I walk into my doctor’s office, demanding an induction – all the while, knowing all the risks of doing such – my doctor doesn’t want to lose me as a customer, so he agrees.
You Have More Power Than You Know
On the flip side, if more women – more consumers – are asking their doctors to allow their bodies to go into labor naturally, they will stop suggesting and allowing for non-medical inductions. If more women are getting educated on their options and on the pros and cons of such procedures, and refusing inductions for the sake of convenience, doctors will follow suit. Ultimately, they want to make their customers happy.
For more information on inductions, please visit MedLine Plus, American Pregnancy Association, and the Adventures of a Labor Nurse.
"Amniotic fluid peaks at 34 weeks, reaching around 800 mL, and gradually declines to around 600 mL by 40 weeks." - tweet this!
Related articles:
Knowing Your Options Is Vital To Your Labor And Birth
How To Avoid a C-section Without Changing Hospitals
6 Comfort Tips For NOT Breastfeeding
So You Need An Induction, Eh?So You Need An Induction, eh?
I believe women (actually any person) should be able to whole-heartedly trust their doctors. We want to believe our doctor is doing what is in our best interest – and they should be.
by Lauren King, Registered Nurse, Certified Lamaze Educator, and DONA Labor Doula
Photo By BirthYearBook
I feel the need to provide a disclaimer before I delve into this topic. I am not saying all doctors, midwives, or other medical staff are bad. There are definitely a lot of really great medical personnel out there. But just like anything in life, there are always a few bad apples.
I believe everyone should be able to whole-heartedly trust their doctors. We want to believe our doctor is doing what is in our best interest – and they should be. But I don’t think it’s a secret that there are doctors that sometimes do things in their own best interest. The question is: how do you know? As a non-medical person, how does one know their doctor is top-notch, and not suggesting every intervention, hoping for another nickel in their pocket, or hoping to be out on the golf course in an hour?
Of course, the obvious response here is: talk about your options with your doula from The Happiest Doulas, and we will do everything we can to help you achieve the beautiful birth you want and deserve. But equally as important is to be educated. You don’t need a nursing degree or a medical license to make important medical decisions, but you do need at least a pretty basic understanding of some of the top decision areas. And for everything else, ask lots of questions. Specifically, discuss the B-A-R with your provider: benefits, alternatives, and risks. When discussing pros and cons about procedures (especially induction) a great question for your provider is, “What research do you have about that topic?” or, “Where can we get more research-based information about that to help us make a decision?”
I’ve written before about inductions, but this is a topic that comes up a LOT in my classes. Plus, it’s the topic that really gets me started, gets me up on my high horse, my soap box… and it is hhhaarrrddd for me to get off it! “My doctor wants me to have another ultrasound next week because the baby is measuring big,” – and as a bonus to that one, “And if I don’t deliver by my due date, the doctor wants to induce me.” “My doctor said my amniotic fluid level is low.” “My doctor told me I need an induction because I conceived through IVF.” Ok, well, I don’t actually know what the literature says specifically about IVF, but just in my personal OPINION, it doesn’t make sense to me.
"I whole-heartedly believe in inductions for medical reasons for mom or baby’s health." - tweet this!
Let’s talk about the reasons for induction, though. There are actual medical reasons for induction, and I whole-heartedly believe in inductions for medical reasons for mom or baby’s health. What I don’t believe in is disguising a convenient induction in medical terminology. Here are some medical reasons for induction, according to ACOG: pregnancy that continues 1-2 weeks past the estimated due date, high blood pressure, uncontrolled gestational diabetes, an infection in the uterus, or a baby who is not growing properly (IUGR). This list is not completely exhaustive, but “big baby” and even “low amniotic fluid” (by itself) are not included in the list of medical reasons for induction.
I’ll discuss those two things in a later post, but for now, let’s discuss induction for postdates (going past your due date). Do you know what “EDC” or “EDD” stands for? Both start with E for estimated. (EDC stands for “estimated date of confinement”, in case you didn’t know.) A point I made in one of my classes recently was this: do you always have a 28-day cycle? Do you know, for a fact, that you ovulated on day 14 when you got pregnant? Do you know, for a fact, the exact date you conceived? (Ok, so some can truthfully say ‘yes’ here.) So, I went on to say: Did you all walk at 12 months? Did you all crawl at 7 months? Did you all roll over at 3 months? My point is that just as we all grow and develop at different rates Earth-side, so too do our babies grow and develop at different rates in the womb.
Due dates are calculated based on an archaic formula, called Naegele’s Rule, which assumes every woman has a 28-day cycle. Even then, the man behind Naegele’s Rule, Frederich Naegele, was not the original “inventor” of “how to estimate the length of human gestation.” It was an 18th-century professor of botany and medicine, Hermann Boerhaave, who developed the formula. Am I the only person who thinks this whole business of calculating a due date deserves a little more visitation by the research and medical community?!
Many Are Mislabeled as "Post-Term"
I do a lot of reading to keep up with the newest information. One of my favorite places to get information is from Evidence Based Birth. Rebecca Dekker, the author, just published a very extensive article on the evidence for inducing for going past your due date. She touches on Naegele’s Rule as well, but one thing she wrote really struck me. She wrote, “using the LMP [last menstrual period] to estimate your due date makes it more likely that you will be mislabeled as “post-term” and experience an unnecessary induction.” The reason for this is just as I stated above: not everyone’s cycles are cookie-cutter perfect! Even if a woman does ovulate on day 14, if she conceives that month, the embryo may not implant for several days! I was so thrilled for this article to come out, I wish everyone could take the time to read it word-for-word; however, I realize it is lengthy. I encourage you to skim it, and if nothing else, read the section “What’s the bottom line?” found at the end of the article.
"If a woman ovulates on day 14, and conceives that month, the embryo may not implant for several days." - tweet this!
So that you have more time to read that very important article, I’ll go ahead and end now. I hope this has given you some valuable information and resources. Next up, I’ll discuss why doctors induce for “big baby” and low amniotic fluid, so come back soon!
7 Tips to Better Organize the Nursery Now!
Simplify now to reduce clutter (and frustration) later. Colleen Downey, co-owner of Indianapolis Doulas, a full service doula agency serving families in Central Indiana, provides her tips for nursery organization.
by Colleen Downey, Birth and Postpartum Doula
If any of my friends from high school are reading this, I’m sure you’re shocked that I’m the person writing about organization. Because, like, whoa. But alas, my life has led me to this crazy place of being somewhat of an expert in birth, breastfeeding, AND organizing nurseries. So hang on, because here we go.
7 Tips to Keep Your Baby's Nursery Organized and Clean
1. Only keep items you’ll use. In my experience, you’ll need 10‐15 sleepers (maybe a few extra fleece ones for cold nights), 10 onesies, 10 pants, infinite socks (seriously, those little stinkers are always coming up missing), 5‐10 t‐shirts MAXIMUM! Donate or sell anything above and beyond.
2. Use Oxiclean. Seriously, this stuff is amazing at getting all kinds of stains out. For the really bad ones like breastmilk, formula, and blowouts be sure to soak them in the wash with oxiclean overnight and they’ll look like new!
3. Roll everything! You know how you roll your clothes when you pack a suitcase? Same thing with baby clothes. You can see all your options and you don’t have to dig to find them. Anything that is just too bulky to roll hang up in the closet.
4. Plan ahead. Use the dresser for the size your child is currently wearing and the next size up (For example, newborn and 0‐3 months). Keep them separate but easily accessible. Save yourself a headache and use the closet for clothing two sizes up from their current size (in this case, 3‐6 months and 6‐9 months).
5. Have two small laundry baskets in the closet. One for clothes that are too small and one for the clothes that are too big. No matter how carefully you organize, there are always a few stragglers. Having a place to put them helps you keep out the clutter.
6. Have a laundry basket just for your kid’s stuff and wash it separately. Not because you need special soap or anything, just so folding and putting away goes quicker. You’re a parent—you want to save time wherever you can and this is it. Ain’t nobody got time for more laundry.
7. Get a shoe box or a small basket. Use it to contain my arch nemesis—baby socks, hats, bibs, and underwear when they get older.
Simplify Now to Reduce Clutter Later
These tips totally apply to toys and whatever else you got at your baby shower, too. Trust me, your baby doesn’t need much. The sooner you simplify and get rid of unnecessary things the easier your life will be.
Support Your Postpartum Abs with Belly Binding
After childbirth, easily improve your posture, stabilize loosened ligaments, and support the abdominal wall while muscles retract and organs return to their pre-pregnancy location.
Did your body swell and expand during pregnancy? I would be surprised if it didn’t. All mothers experience some form of swelling from retained water, fat and air. This extra cushioning is important to support the baby, mama’s organs and bones. After birth, when this extra cushioning is no longer needed, her body will naturally start to shrink back down to her pre-pregnant size. Belly binding may speed up this process and provide support to women during their recovery period.
What is Bengkung Belly Binding?
A belly bind gives full support to a mother’s abdomen, torso and pelvic area. This helps to improve posture, stabilize loosened ligaments and support the abdominal wall while muscles retract and organs move back into their correct place.
The pelvic floor is a huge support system for your bladder, colon and lower intestines, and support is crucial as the cervix needs to shrink and muscles need to heal without stretching further. Have you ever wondered why so many women experience incontinence after giving birth? Why a cough, laugh or sneeze makes you stop and wonder what just happened!? The pelvic floor can remain unstable for several months after giving birth – any extra support in this region is readily welcome by most women.
Hips need to close and the constant pressure from the bind can help support this. Binding can aid in the healing of ailments like diastasis recti (the separation of your outer most abdominal muscles), and in more extreme cases can be used in tandem with certain strengthening exercises recommended by a Physical Therapist.
Spine and posture realignment are commonly needed as pregnancy has a tendency to throw things out of whack. As babies grow in utero, it shifts moms balance by tipping the pelvis forward and the tailbone backwards, and ultimately both the lower and upper spines compensate for these changes and mom is left with the classic “S” shaped spine, which causes aches, pains, and weaknesses. The added support of a bind is often a gentle reminder for mothers to be cautious of their posture, as some women tend to hunch over when picking up babies or even while breastfeeding.
When To Wrap Up
Belly binding can also be used by those who have had cesarean births. Binding can start between 4-6 weeks postpartum for a mother who is recovering from a c-section and for those who’ve had a vaginal birth, start a few days postpartum. It can be worn for a few days or up to 6 weeks.
When looking for belly binding information to share with you, I came across this post from a chiropractor at Core Exercise Solutions about diastasis recti (abdominal separation). The author reviews both the pros and cons of belts like the Belly Bandit type, which is a commonly used product available in many different sizes/styles. I think the points made in the post also apply to the Bengkung Binding method.
Finally, I found this virtual service for learning how to wrap safely. The site includes a shop for the needed supplies, which makes me want to try it out! (Non-affiliate link.)
Stillbirthday: Waiting For His Cry
Experiencing loss anytime during pregnancy is one of the hardest things anyone can face. One mom shares how she lost but overcame, and tells her story as part of her healing and to raise awareness of Stillbirthday.
In 2010 I was expecting our second baby, a little boy named Weston. My pregnancy was just like my first, easy and nothing out of the ordinary. I finally got to 39 weeks and was anticipating birth any day. One Sunday, I remember telling my husband I hadn’t felt the baby move a whole lot that day, but I didn’t think anything of it because you always hear people say babies don’t move a whole lot at the end because there’s not much room left. I went through the following day, still not thinking much of movement. I stayed busy with my toddler and my other two adopted kids and never really stopped to count kicks.
The next morning, I had an appointment with my home birth midwife and during the 45 minute drive, I kept pushing on my stomach to see if the baby would kick me back, but there was nothing. Deep down I knew something wasn’t right, but I still didn’t think the worst and was actually a little excited because I had started feeling slight contractions during the drive. I came into my appointment and told my midwife how I hadn’t felt a lot of movement and she wasn’t overly concerned at first either. We got to the point of the heartbeat check and she tried for several minutes, but couldn’t hear it. She said I should go straight to the hospital where they could do an ultrasound to determine what happened.
As I drove to the hospital I called my husband and best friend to tell them what was going on and to meet me at the hospital. I was checked in and sent down for an ultrasound right away, where they determined my baby had no heartbeat. I think I was in shock because I was abnormally calm and went back up to the delivery floor to be admitted. I’m typically a very natural birther, but this time I decided to have the epidural so I wouldn’t have to face the birth pain as well as the pain of not having my baby to take home at the end.
Since I was already in early labor, I was able to get the epidural fairly quickly and relax until it was time to birth my son, about 6 hours later. The nurses had previously asked me if I wanted to hold him right away or have them take him and clean him up a little bit before they gave him to him. At the point when they had asked, initially I had said to clean him up and bring him back, but when he was born, I changed my mind right away and asked them to hand him to me as he came out.
It was a surreal experience holding my still baby. I kept waiting for his cry, but it never came. I held him for quite a while and studied his perfect features, trying to remember the baby I wouldn’t get to watch grow up. I was surprisingly not that emotional at first. It wasn’t until later that night when we were able to be discharged that it hit me; I would not be bringing my baby home with me. As they pushed me down the corridors of the hospital to our car outside, I cried and continued to cry all the way home.
I don’t remember much from the rest of that night. It was late when we got home, so I think we just passed out and slept until morning. Morning felt like we had just been through a dream, but the realization of my lost baby hit hard, especially as family started to come into town for support.
A day or two after the birth, we went to the funeral home to prepare for our son’s funeral and burial. That was another surreal moment in my life. You picture yourself “someday” being in the funeral home planning a funeral for your parents or elderly loved ones, but you are never prepared to be in the funeral home talking with the director about your tiny baby born just days before.
We had a very nice, small graveside ceremony with close friends and family and buried our angel in a special part of the cemetery called “The Angel Garden” set aside for young children and babies.
While still in the hospital, the nurses told us about the photography group, Now I Lay Me Down to Sleep, who come to the hospital and take photos of stillborn babies as a way to keep their memory alive. I’m so grateful to the photographer who captured our angel for our memories. What a heart-wrenching, but fulfilling job these photographers must have! We were able to use the photos to make a photo book and share with our other kids since they did not actually see their little brother (we thought they were a bit too young to deal with that at the time).
We ended up getting pregnant a couple months later with my daughter and looking back I honestly don’t remember what it was like the months following our loss. People kept telling me, “You’ve all dealt with your loss with such grace and maturity.” So I guess we must have handled it “well” in others’ eyes. I guess for us, while we definitely questioned why, we never had “anger toward God” like some may experience during a similar loss. As the years have gone by, we still think about and miss our angel. I always wonder what he would have been like and what he would have become. Dealing with our loss has been the hardest thing I’ve ever had to experience in life so far. However, it really was our faith that got us through it and how I’m able to share our story to this day. Even though we may never understand, we trust that everything happens for a reason and that God is in control.
If you need support during your experience with loss, consider the organization, Be Not Afraid. Their group offers peer-based support to parents experiencing a prenatal diagnosis and carrying a pregnancy to term.
Related articles: Know the Symptoms of Postpartum Anxiety and Depression Doulas Provide Support Through Life and Loss
Doulas Provide Support Through Life and Loss
An open letter from a certified bereavement doula to other doulas dealing with loss. Statistically speaking, every doula will likely encounter the death of a client's baby. This is how you can help those clients, and yourself, grieve for that loss.
by guest blogger, Sarah DiMarco
An open letter from a certified bereavement doula to other doulas dealing with loss. Statistically speaking, every doula will likely encounter the death of a client's baby. This is how you can help those clients, and yourself, grieve for that loss.
One in every 160 babies are born sleeping. One in every four pregnancies ends in miscarriage. The reality of these statistics is that eventually, as doulas, we will all experience the loss of a client’s baby. For me, I’ve been practicing as a doula less than a year, and my first professional experience with loss was during my third birth. That loss was what prompted me to train with Stillbirthday. I wanted to be able to share my training and experience so that I can help you, sweet doula, if you have found yourself in a place that you are unprepared for.
Filling the Space Where Birth and Bereavement Meet
After receiving the news that their baby will not make it, there are many things that must happen next for the parents. Many well meaning obstetricians, nurses, and midwives think to ease the family’s grief by making these decisions for them. For example, if a couple has been told at 36 weeks gestation that their baby has passed away, a midwife may think that it would make things easier on the family to induce labor as soon as possible, but in many cases, it can be safe to continue to carry the baby until labor begins on its own. Choosing to do so can allow the parents time to come to terms with the news and make plans and arrangements for the welcoming and farewell of their baby.
Just as it is your job as a birth doula to provide the expectant family with options, choices, and resources; it is your job as a bereavement doula to do the same. The death of a baby does not mean that those options and choices are taken from the pregnant or laboring mother but sometimes she needs a gentle reminder of this fact. In truth, the role of a bereavement doula is very similar to the role of a birth doula.
When Hello Becomes Goodbye
But of course, there are parts of being a bereavement doula that differ. It’s a difficult but important part of your job to help the family transition from welcoming their baby into the world, and telling him farewell. Even if their baby is born sleeping, his birth can be a beautiful and even joyful experience for the mother and father. It should be your goal to remind them that they have given birth and they are parents.
It’s also important to preserve the memory of their baby’s birth. Encourage parents to have a photographer, such as one from Now I Lay Me Down to Sleep (NILMDTS) to take pictures of their baby and of themselves, as well as older siblings or other family members holding her. If the family seems apprehensive about this you can offer to show them photos from the NILMDTS website and give them time to decide. If they have chosen to have a photographer come, it can ease their minds if you offer to stay in the room, perhaps behind the curtain or just inside the door to give them privacy. This way, if you sense they are overwhelmed with their grief, you will be there to provide comfort or ask a nurse to take the baby back.
A doula can help walk the family through the process of planning the farewell ceremonies. If you are unfamiliar what that process is, you can just be there to provide support while the parents make the difficult decisions on what to do with their baby’s body. Often, just sitting quietly and being there with the family is the only thing you can or need to do.
It’s also so important for a doula providing support to families during loss to know what NOT to say or do. Things such as “you can always try again” or “God has plans” are said with the intent of comforting, but they can do just the opposite. Also, any phrase that starts with the words “at least” is not going to be as helpful as one would think.
The most important thing to remember when you’re providing support to families enduring loss is to allow yourself to grieve as well. Don’t hold back your emotions in front of your client to be “strong” for them because it is actually comforting for the parents to see that their baby’s life touched others. If you need to, pause and take a moment for yourself during the labor and birth to collect your thoughts and check-in with your mind and body.
Be Gentle With Yourself: Self-care is Imperative
Once you’ve arrived home after the birth, take a warm bath with pretty candles and a hot cup of tea, do some yoga, or sit with a good book. You must remember self-care and to allow yourself time to grieve. It’s important to debrief with a trusted doula-friend, family member, or therapist, so that you may heal and continue to provide support for the families you work with.
As doulas, we are truly unique women. We have chosen a path that requires much love and compassion and we all have that inside of us. You are already equipped with exactly what you need to provide the support your clients need, in any birth outcome. You are amazing. You are valuable. You are needed.
Sarah is a mother of five children; two step-daughters ages 16 and 8, a 5 year old daughter of her own, and two angel babies born in the first trimester on September 2, 2013 and March 8, 2014. Sarah is a certified Stilbirthday Birth and Bereavement Doula, and a MotherMe Graduate Birth and Postpartum Doula. For more info about Sarah and her life's work, please visit her website.
Tap Your Fears Away!
EFT, or Tapping, is a method of reducing and eliminating negative emotions such as fear, anxiety, shame and anger.
by Cynthya Dzialo, Certified CBI Birth Doula and Hypnobabies Hypno-Doula
Emotional Freedom Technique (EFT) or Tapping, is a method of reducing and eliminating negative emotions such as fear, anxiety, shame and anger. The process is quick, painless and simple to learn, with permanent results. The theory is that an imbalance has occurred in the body due to an energy disturbance, which can be corrected by tapping on the meridians to clear away the negative emotions. It is easy to do and takes little time. You'll feel better so try it out.
““The cause of all negative emotions is a disruption in the body’s energy system””
Clearing the Energy Disturbances
EFT works by intentionally activating an energy disturbance by thinking about a painful memory or just feeling your feelings. While the energy disturbance is activated, you tap with your fingertips on a set of 10 easily learned acupuncture points in order to clear out the energy disturbance in the affected meridians. As the disturbance gets cleared through the tapping, you will experience your negative emotions actually drain away. When the energy disturbance has been completely cleared, your negative emotions will be gone. You can then think about the memory with no painful emotional reaction! Problems in your life that resulted from the original experience will clear up as well.
It's Important to Stay Focused on the Problem While Tapping
It is essential that the energy disturbance remains activated the whole time you are tapping in order to completely clear it. Therefore, you have to keep your attention focused on the negative feelings while tapping until they are gone. Getting distracted or thinking about two things at once can interfere with EFT working.
5 Must Try Morning Sickness Remedies
Take comfort in knowing most women find morning sickness cures itself by the time they begin the second trimester of pregnancy.
Do you have morning sickness? It is caused by hormonal changes, vitamin deficiency, low blood sugar, strong smells and typically tends to get a little worse around the 12th week or so. Here are a few natural remedies that can get you to the homestretch!
1. Try sipping ginger "tea." Take a fresh root of ginger and grate it, or slice it into slivers and drop into a cup of boiling water. Or, if you’re in need of some quick relief, you can put it into a mug and nuke it for about three minutes. Add a little honey to taste and drink every morning!
2. Try boosting your intake of Vitamin B6. Several studies have shown that vitamin B6 supplements reduce nausea in pregnancy. Spinach, sunflower seeds, potatoes, chicken and whole grains are all good sources, along with nuts, peas, and beans.
3. Have a snack or nibble on something every few hours to avoid low blood sugar, which can trigger nausea and vomiting when pregnant.
4. Stay hydrated. If even mildly dehydrated, you may vomit more. It’s been found that women who drink a glass of water every hour are much less likely to suffer from morning sickness, so bottoms up!
5. Potato chips. I know, I know. This one is definitely a little off the beaten path, but potato chips can alleviate nausea that’s due to over-production of saliva. The salt present in potato chips helps dry up the saliva.
They Say It's Temporary: Sick of Being Sick
Morning sickness isn't fun, but it's temporary. If none of these cures work for you, take comfort in knowing most women find morning sickness cures itself by the time they begin the second trimester of pregnancy.
Related articles:
Nutrition Tips For Thriving During Postpartum
6 Points to Consider When Hiring a Labor Doula
Happy Mama = Healthy Baby
Relieve Nausea, Reflux and ConstipationKnowing Your Options is Vital to Your Labor and Birth
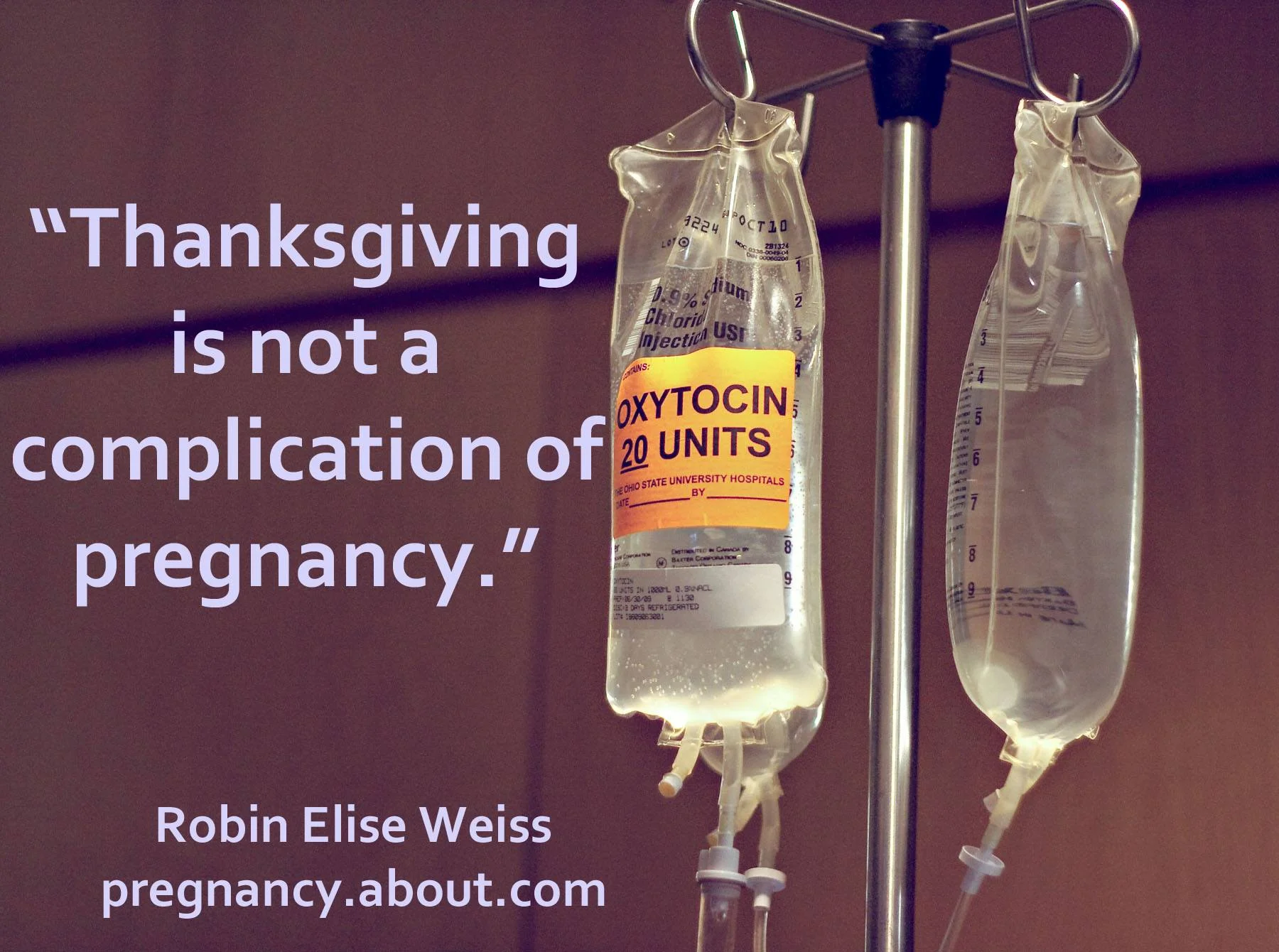
I’d also be willing to bet that your doctor has casually mentioned scheduling an induction. It would be convenient to have a baby before all the craziness of the holidays really settles in, wouldn't it?
by Lauren King, Registered Nurse, Certified Lamaze Educator and DONA Labor Doula
Are those adorable “Mommy’s Little Turkey” outfits staring you down as you walk by in the store? You bet! Are the Christmas carols playing at Target yet? Of course! Is your financially-savvy hubby hoping for that tax write-off to arrive before the New Year? Definitely!
I’d also be willing to bet that your doctor has casually mentioned scheduling an induction. You know, so you can be home in time to enjoy the holidays with your family. Or maybe that thought already crossed your mind. It would be convenient to have a baby before all the craziness of the holidays really settles in, wouldn't it? But that’s the problem. It’s convenient. Let that sink in for a minute. Convenience. Who benefits from this convenience? Let me give you a hint: it ain’t you, and it ain’t your baby either. When asked by your doctor if you’d like to schedule your induction, be sure you are honestly weighing the risks and benefits. Induction puts you at a greater risk for c-section, and it also puts your baby at greater risk for health concerns if she is not ready to be born yet.
Give your baby and your body the chance to go into labor when the time is right naturally, not conveniently. I promise you, that is the best gift you will receive this holiday season, and some things are definitely worth waiting for! Do your research, and know your options - a doula can help you find unbiased, and well-rounded information. Don't miss out due to the hectic holiday schedule - schedule an interview today with one of The Happiest Doulas before she is booked.
Related posts:
Childbirth Classes Prevent Birth Trauma
5 Labor Tools for Partners
Consider Hiring a Labor Doula
Make Labor ProductiveThe Perfect Swaddle in 5 Easy Steps
For many months your baby has been "swaddled" in a luxurious, comfortable haven where everything is perfect for her wellbeing. Learn to replicate this feeling after she is born.
Swaddling is one of the oldest tidbits of wisdom for helping babies sleep better. Most new parents hear this advice from someone they know, yet some are hesitant to try it or say they have tried it and "my baby doesn't like it." Saying that a baby doesn’t like swaddling is like saying traffic isn’t bad at 5pm on a Friday in Atlanta! A baby NEEDS swaddling for at least the first 4 months of life, sometimes longer. Recreating the womb by swaddling will help transition your baby into the world.
For many months your baby has been "swaddled" in a luxurious, comfortable haven where everything is perfect for her wellbeing. Especially in those last few months, your baby is packed very tightly inside the womb and by 40 weeks, she is very used to the wonderful feeling of protection around her.
Parents often think babies need and want their hands free once they are outside of the womb. However, it is quite the contrary. Since babies have been tightly packed in the womb for so long, being “free” when they are born often causes fussiness, restlessness and a baby who doesn’t sleep very well. Give them a tight swaddle and it can make a world of difference!
First, you'll need a large square blanket (40in x 40in cotton flannel blend fabric work the best) to swaddle with.
Second, you'll need to use the perfect method. Here's how to swaddle in 5 easy steps:
1. Start by laying the blanket down in a diamond shape on a nice flat surface such as a bed. Fold one corner of the blanket down several inches. Lay the baby with the back of her neck along the fold.
2. Be sure the baby’s arms are straight to the side and snugly wrap the left side of the blanket completely over the baby and tuck it under her body on the right side.
3. Take the very bottom point of the blanket (below the feet) and bring it up just enough to tuck under her left shoulder (which would be her shoulder on your right). It’s ok to leave a lot of space near the feet.
4. Make sure her other arm is straight to her side and fold down the top right corner of the blanket and bring it to the middle of her chest, leaving the excess material out to the side. This will create a small fold on the baby’s chest that you can tuck the “tail” of the blanket into in order to keep the swaddle nice and tight.
5. While holding the fold in the middle of the chest, take the excess material, grab it in a bunch and wrap it snugly the whole way around the baby’s arms.
To be sure your baby is swaddled in a hip healthy way, the legs need to be free to move about. Be sure your baby can move his legs into a “frog like” stance while inside the swaddle by holding his feet in your hands and gently pushing them toward his body so his knees splay outward in a “frog like” stance. The blanket should be loose enough around baby’s hips and legs to allow this movement easily, without restriction. This will ensure the hips are not being restricted and will avoid hip dysplasia.
If you want to learn more, arrange now for a private, online lesson for personalized answers to your specific questions and concerns for caring for baby. You can review the details of all of our online parenting and feeding classes here.
Bookmark this article for future reference and if you've found these tips useful, please share this post with other new parents. I hope this helps you jumpstart your way to having the happiest baby on the block and a restful night's sleep.
Shhh! A Baby’s Language of Love
A quiet atmosphere often makes babies fussy and sleep in shorter stretches between feedings. Try our recommendations!
Shhh! Who could have known the same sound that speaks of annoyance to an adult could speak in a whole other language to a baby’s ears? Most adults automatically “shh, shh” a baby when it’s crying, but what most of us don’t realize is by speaking in “Shhh language” we are actually speaking a language of love to our babies.
During your first trimester your baby develops ears and is able to hear sounds inside and outside the womb. What most parents are unaware of is exactly what a baby is hearing inside the womb and at what intensity this sound is.
The blood rushing through your arteries creates a continuous shhhing sound. This sound is about two times louder than a vacuum cleaner! You can imagine how quiet it seems to a baby once it’s born when everyone is tiptoeing around for fear of waking the baby. Having such a quiet atmosphere often makes babies fussy and sleep in shorter stretches between feedings.
So you may be thinking, what is the solution? A white noise (sound) machine will become your new best friend. Sound Therapy, made by Conair, can be found on Amazon.com for $17-25. The Conair brand is a personal favorite because it’s inexpensive, but works like a charm.
Key points to get the best out of your noise machine:
Turn it up as loud as possible. It should be about as loud as your vacuum cleaner.
Place it 2-5 feet away from the baby’s crib.
Make sure it plays continuously through the baby’s sleep time at night and naps (the Conair brand may have a timer button on the side - make sure this is OFF).
One more thing - if you don’t have access to a noise machine in a public place such as a store, you can use your own shhhhing. Again, be sure it’s loud (at least as loud as the baby is crying) and place your mouth about 2-4 inches from the baby’s ear so she can hear you. You may worry about how many rude stares you will receive, but then be surprised at how many “Wow’s” you get once people see your baby quiets down in a matter of seconds! View the video below of shhhhhing and see for yourself how well it works!
Bookmark this article for future reference and if you've found these tips useful, please share this post with other new parents. Hope this helps you jumpstart your way to having the happiest baby on the block and a restful night's sleep.
Why I Left Labor and Delivery to Be a Doula
I was getting burned out on the number of women coming in for inductions for all the wrong reasons, or worse – they didn’t even know why they were being induced.
by Lauren King, Certified Lamaze Educator and DONA Labor Doula
A lot of clients ask why I left the hospital bedside as a labor and delivery nurse to become a doula. There are two main reasons: one is because I am so very passionate about educating women about labor and delivery. As a nurse, I was tasked with charting, charting, charting, fetal monitoring, charting, following policies, calling doctors, giving medications and MORE charting! If I had the joy of answering many, many questions for a patient and her family, then something had to suffer – usually my charting.
Aside from educating my patients, I loved being there for them. I loved that bond with my patient and her husband, family or friends that were there by her side. Though the nurse-patient bond can be special, at the end of my shift, I went home. Whether the patient delivered her baby or not, it was time for me to go! Yes, sometimes I stayed late if a patient was close to delivery (and luckily, our charge nurses were generally very understanding in those situations), but then I’d “drop and run,” leaving my beloved patient in the hands of my night-shift colleagues. And I’d most likely never see that patient again. Becoming a doula was a way for me to ditch the charting, BE with my patient (now my client!) and provide education.
Doctor Knows Best: Burn Out is Real
Which brings me to my second reason for leaving the bedside: I was getting burned out on the number of women coming in for inductions for all the wrong reasons, or worse – they didn’t even know why they were being induced. They just didn’t know. They didn’t educate themselves! They thought, “Well, my doctor said I need to be induced now, so I should trust him/her. Doctor knows best! And I certainly don’t want to hurt my baby.”
“So many of these women wound up having a cesarean section, and sometimes I felt like I failed them.”
So many of these women wound up having a cesarean section, and sometimes I felt like I failed them. I failed to educate them on their options. I failed to tell them they don’t have to be induced just because “their” doctor is on call! I failed to encourage them. I failed to move them enough if they had an epidural. It’s not that I didn’t care – sometimes my patient flat-out didn’t care what I had to say. Or maybe I was just too busy with my other patient. Or perhaps, I had that very rare moment when all seemed well enough for me to use the restroom or go eat, and upon my return – BAM. C-section was called while I was gone. Ugh! If there’s one thing I hated as a nurse, it was an induction for non-medical reasons, or inductions for fake medical reasons (baby “too big,” anyone?). Especially if it ended up in a c-section.
There are, of course, other reasons for my leaving the nursing world. Don’t get me wrong – I loved my job and I loved the hospital where I worked. I also loved the other nurses I worked with. Nursing burn-out happens, and unfortunately, it happened for me in my favorite field of nursing. But, the good news is: there are plenty of options, and becoming a doula and a childbirth educator are right up my alley!
Related articles:
Investing Your Time in Childbirth Education
AROM: To Break or Not To Break
5 Reasons to Hire a Birth Doula
Postpartum Expectations and Must-have Items